Lifestyle Changes Outperform Pharmaceuticals in Treating Vaccine Injuries and Long COVID: Survey
Lifestyle changes may be more effective than pharmaceuticals in treating long COVID or post-COVID vaccine syndrome, preliminary survey findings suggest.
Over 450 individuals who identified themselves as vaccine-injured were surveyed on treatments they found helpful. Treatments were then ranked based on the number of patient reports.
While only vaccine-injured individuals were surveyed, the similar symptomatology and disease mechanism between long COVID and postvaccine symptoms means that the same therapeutics may be applicable to treat both conditions.
The data were presented by Dr. Joel Wallskog, co-founder of React19, an alliance dedicated to supporting individuals affected by such conditions, at the Front Line COVID-19 Critical Care (FLCCC) Alliance conference on long COVID and vaccine injuries held in April.
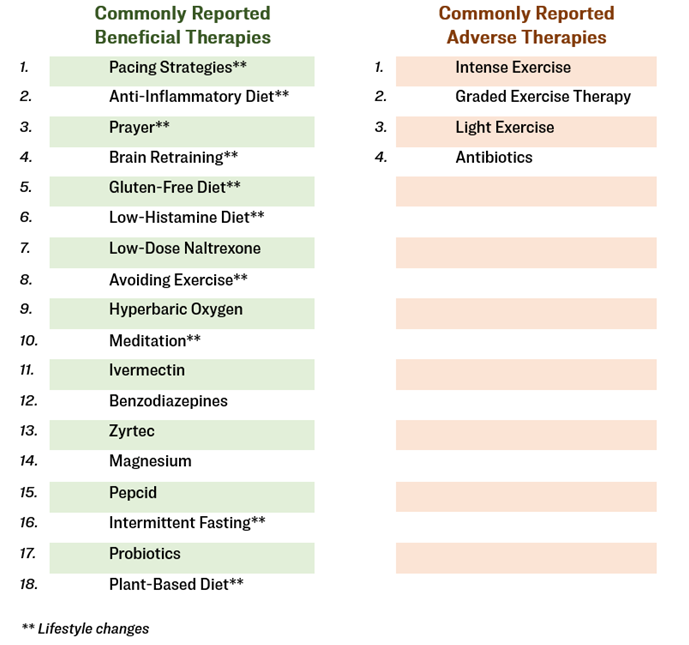 React19 survey findings. Lifestyle changes are labeled with asterisks. (The Epoch Times)
React19 survey findings. Lifestyle changes are labeled with asterisks. (The Epoch Times)
Pacing Strategies
Pacing strategies have emerged as the most effective change for managing symptoms.
Unlike healthy individuals, those with long COVID or vaccine injuries often experience chronic fatigue daily. It’s as if they have limited energy reserves, and even simple tasks like showering or walking the dogs can quickly become exhausting.
To prevent burnout, people in this condition must pace themselves and carefully plan their activities to ensure overall functionality and well-being, Wallskog told The Epoch Times.
Physical therapies are often considered the opposite approach.
Unexpectedly, findings from the React19 survey revealed that all forms of exercise seemed to exacerbate symptoms, with avoiding exercise ranking as the eighth most helpful therapy for symptom reduction.
Wallskog, an orthopedist, noted the tendency among doctors in his specialty to recommend physical therapy when uncertain about treatment options. However, the survey’s data serve as an educational reminder for doctors not to rely on physical therapy as a knee-jerk response.
“It’s counterproductive in this population,” Wallskog said. Reflecting on his own experience, he admitted to attempting regular workouts and therapy sessions, only to find himself almost bedridden for an entire week afterward.
Fasting May Clear Spike Proteins
Scott Marsland, a nurse practitioner specializing in long COVID and vaccine injuries, and Dr. Syed Haider, a board-certified internist, suggest that intermittent or prolonged fasting can be an effective lifestyle change for managing vaccine injuries and long COVID.
Fasting offers several benefits besides weight loss, including improved cognition and reduced inflammation and oxidation. It can also activate autophagy, which may aid in the removal of COVID-19 spike proteins, Marsland said.
The FLCCC, one of the leading health practitioner organizations treating long COVID and vaccine injuries, believes that spike proteins, whether from the infection or the vaccine, play a significant role in patients’ symptoms, including fatigue and cognitive impairment.
“The spike protein, notably the S1 segment, is likely the major pathogenetic factor leading to postvaccine syndrome,” reads the FLCCC protocol on treating COVID-19 vaccine injuries (pdf).
Studies have shown that the COVID-19 spike protein can induce inflammation, microclotting, mitochondrial dysfunction, autoimmunity, and neurological damage, leading to a complex of symptoms, including fever, shortness of breath, fatigue, brain fog, and many more.
During fasting-induced autophagy, spike proteins can be broken down along with other unused or foreign proteins. Marsland said that prolonged fasting aims to activate chaperone-mediated autophagy, which specializes in protein degradation and typically peaks after 24 hours of fasting. Thus, prolonged fasting for at least 72 hours per session is often encouraged.
While there is no definitive test to confirm the removal of spike proteins through fasting, patients who diligently follow fasting protocols often show lower anti-spike antibody levels, indicating potential removal of spike proteins, Marsland added.
In addition to clearing spike proteins, fasting can reduce inflammation. According to Marsland, some patients experience improved brain fog during the later hours of a 72-hour fast.
Haider noted cases where patients had experienced complete symptom reversal during fasting. Patients can begin with a 12-hour fast overnight and have a 12-hour feasting window during the day. Once accustomed to it, they can gradually increase fasting hours to 16 hours with an eight-hour feasting window. However, it is important to consider individual needs and preferences when determining the fasting schedule.
Fasting Not Recommended for Everyone
Fasting can come with various drawbacks, such as mood swings, nutritional deficiencies, blood sugar imbalances, and loss of muscle mass. For those who want to do prolonged fasting regularly, Marsland cautioned that patients should stick to 72-hour fasting sessions at a maximum of once per month. This schedule is important since some people may lose muscle mass and, in rare cases, muscle wasting.
People with diabetes or those taking medication should consult their doctors before starting a fasting regimen. In addition, pregnant and breastfeeding women are advised to avoid fasting.
Dietary Changes
People with autoimmune diseases, gut dysbiosis, or mast cell activation syndrome resulting from long COVID or postvaccine syndrome may find relief and reduce inflammation by following low-histamine and noninflammatory diets.
Brianne Dressen, one of the first vaccine-injured patients in the United States and the co-founder of React19, said her low-inflammatory diet has been a “game changer” in controlling her postvaccine mast cell activation syndrome.
Addressing excessive inflammation and hyperactivation as initial steps in treating long COVID and vaccine reactions is crucial, said Dr. Keith Berkowitz, a board-certified internist. Dietary changes play a significant role in reducing background inflammation. Potential dietary modifications include eliminating sugar, processed food, gluten, and dairy. High-histamine foods like aged meats, fermented foods, and dairy can also be avoided, according to Berkowitz. Patients should tailor their diet based on their specific conditions.
Proper hydration is crucial for fluid balance and recovery. Berkowitz said he encountered several patients with dysregulated blood sugar after vaccination. Dehydration is associated with poor blood sugar regulation, and replenishing fluids allows the body to return to normal function naturally.
Stress-Relieving Activities
Stress, whether mental or physical, is common in individuals with long COVID and vaccine injuries. Chronic stress leads to chronic inflammation, causing continuous damage to the body.
To counter stress, the body needs to activate the parasympathetic nervous system, responsible for rest and recovery, instead of the sympathetic nervous system associated with the fight-or-flight response.
Temperature treatments involving cold and heat exposure can help reset the body’s response to external changes and reduce stress. For example, cold water baths and ice can release built-up stress and reduce inflammation, even with minimal temperature differences, according to Haider. Warm exposures, like saunas or warm water baths, offer similar benefits but may not be suitable for individuals with mast cell activation syndrome due to potential flares from heat exposure.
Mindful activities such as prayer, meditation, and being in nature activate the parasympathetic nervous system and promote well-being.
However, not all mindfulness activities are healing. Some have characterized cathartic activities like swearing and listening to heavy-metal music as mindfulness activities. While these may provide temporary relief, they may cause harm instead of improving health. For example, studies suggest that cells exposed to heavy-metal music produce more damaging oxidants than those exposed to classical music.
Lifestyle Changes Are Just 1 Piece of the Puzzle
While lifestyle changes can bring long-term symptom relief for many individuals, they may not provide a complete recovery solution, Dressen said. She found a combination of daily intravenous immunoglobulin infusions and avoiding high-histamine foods to be the most effective in managing her own postvaccine symptoms.
“It’s not as simple as saying, ‘I’m going to meditate and pace myself,'” she said. “If it was that simple, we wouldn’t all be crying out for help over and over.”
Dressen highlighted that lifestyle changes are often prioritized because they are accessible, and more people try them, increasing the chances of positive outcomes.
Additionally, some people have found other therapies, such as hyperbaric oxygen and intravenous immunoglobulin, highly beneficial. However, these therapies can be expensive and less accessible, which may explain their lower ranking.
Wallskog, who has not been very responsive to recommended therapies, said that gaining a new spiritual perspective on his work has been most helpful in coping with his symptoms.
“I think we’re fighting a bigger battle,” he said. “This isn’t just about our adverse events to shots; I think that there’s just a much bigger-picture battle going on.”





.png)


Comments
Post a Comment