Long COVID Treatment Protocol (2023)
The survey’s results mean that over 18 million adult Americans are currently experiencing symptoms of long COVID and 15 million have problems performing daily activities because of it.
The presence of spike protein has been strongly linked with long COVID. Studies have shown that spike proteins are often present in symptomatic patients, sometimes even months after infections.
As we learn more about post-COVID syndrome, however, the definition has been refined to be more accurate and useful:
- Subacute or ongoing COVID-19 (post-acute COVID-19 syndrome): symptoms continuing beyond four weeks from acute infection, up to 12 weeks.
- Post-acute sequelae of COVID-19 (PASC): symptoms persisting beyond the four weeks after acute infection.
- Post-COVID-19 syndrome (long COVID, long-hauler’s syndrome): chronic ongoing COVID-19 symptoms beyond 12 weeks from acute infection.
Long COVID Symptoms
- Long COVID
- Post-acute COVID-19
- Long-term effects of COVID
- Post-acute COVID syndrome
- Chronic COVID
- Long-haul COVID
- Late sequelae
- Post-acute sequelae of SARS-COV-2 infection (PASC)
An international study showed that fatigue is the most common long-hauler’s syndrome, affecting 80% of all patients. Post-exertional malaise affects 73%, cognitive dysfunction affects 58%, sensorimotor symptoms such as loss of smell affect 56%, headache affects 54%, and memory issues affect 51% (R). A year after infection, common persistent symptoms include fatigue (reported by 82% of patients), brain fog (written by 67%), and headache (reported by 60%) (R).
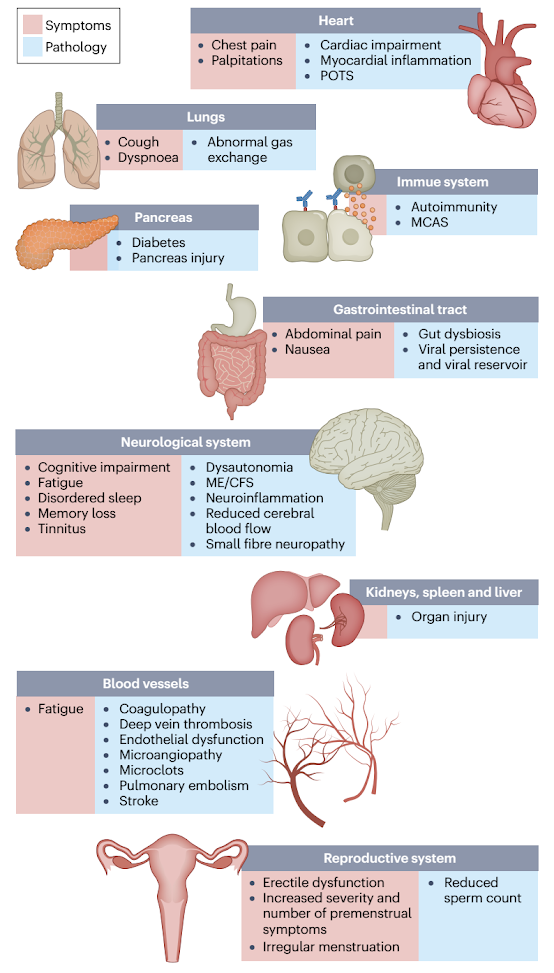 |
| Source: Davis, H.E., McCorkell, L., Vogel, J.M. et al. Long COVID: major findings, mechanisms and recommendations. Nature Rev Microbiol (2023) |
If the symptoms include major shortness of breath, cough with blood in it or pain on one side when you take a deep breath, it could be due to a late pulmonary embolism or a blood clot going to the lungs. Please visit your medical doctor or the nearest 24-hr medical emergency center immediately.
FLCCC I-Recover Protocol
The FLCCC (Front Line COVID-19 Critical Care Alliance) was formed by leading critical care specialists in March 2020, at the beginning of the Coronavirus pandemic, dedicated to developing highly effective treatment protocols to prevent the transmission of COVID-19 and to improve the outcomes for patients ill with the disease.Patients with post-vaccine syndrome should do whatever they can to prevent themselves from getting COVID-19. This may include a preventative protocol (see I-PREVENT) or early treatment in the event you do contract the virus or suspect infection (see I-CARE). COVID-19 will likely exacerbate the symptoms of vaccine injury.
Once a patient has shown improvement, the various interventions should be reduced or stopped one at a time. A less intensive maintenance approach is then suggested.
The core problem in post-vaccine syndrome is long-lasting “immune dysregulation.” The most important treatment goal is to help the body restore a healthy immune system — in other words, to let the body heal itself. Our recommended treatment strategy involves two major approaches:
- Promote autophagy to help rid the cells of the spike protein
- Use interventions that limit the toxicity/pathogenicity of the spike protein
First Line Therapies
(Not symptom specific; listed in order of importance)- Intermittent daily fasting or periodic daily fasts
- Ivermectin (Stone 2022)
- Moderating physical activity
- Low-dose naltrexone
- Nattokinase (Tanikawa 2022)
- Aspirin
- Melatonin
- Magnesium
- Methylene blue
- Sunlight and Photobiomodulation (Red Light Therapy)
- Resveratrol
Second-Line Therapies
- Probiotics/Prebiotics (Lau 2023)
- Vitamin D (with Vitamin K2)
- N-acetyl cysteine (NAC)
- Cardio Miracle™ and L-arginine/L-citrulline supplements
- Omega-3 fatty acids
- Sildenafil (with or without L-arginine and L-citrulline)
- Nigella sativa
- Vitamin C
- Spermidine
- Non-invasive brain stimulation
- Intravenous Vitamin C
- Behavioral modification, relaxation therapy, mindfulness therapy, and psychological support
Third Line Therapies
- Hyperbaric oxygen therapy (HBOT)
- Low Magnitude Mechanical Stimulation
- “Mitochondrial energy optimizer” with pyrroloquinoline quinone, glycophospholipids, CoQ10, NADH, and other nutrients (e.g., Life Extension Energy Optimizer, Restorative Solutions Mitochondrial Nutrition PQQ, Researched Nutritionals ATP 360® and ATP Fuel® and PureEncapsulations Mitochondria-ATP)
- Hydroxychloroquine
- Low-dose corticosteroid
Warning (anesthesia and surgery):
Patients should notify their anesthesia team if using the following medications and/or nutraceuticals, as they can increase the risk of Serotonin syndrome (SS) with opioid administration:
- Methylene blue
- Curcumin
- Nigella Sativa
- Selective Serotonin Reuptake Inhibitors (SSRIs)
About Ivermectin
Ivermectin is a well-known, FDA-approved drug that has been used successfully around the world for more than four decades. One of the safest drugs known, it is on the WHO’s list of essential medicines, has been given over 3.7 billion times, and won the Nobel Prize for its global and historic impacts in eradicating endemic parasitic infections in many parts of the world.
Review the totality of supporting evidence for ivermectin: https://c19ivm.org.
It is likely that ivermectin and intermittent fasting act synergistically to rid the body of the spike protein.It appears that vaccine-injured patients can be grouped into two categories: i) ivermectin responders and ii) ivermectin non-responders. This distinction is important, as the latter are more difficult to treat and require more aggressive therapy.
For ivermectin responders, prolonged and chronic daily treatment is often necessary to support their recovery. In many, if the daily ivermectin is discontinued worsening symptoms often recur within days.
Moving Forward
- List of Doctors that will prescribe Ivermectin and Hydroxychloroquine
- List of Pharmacies that will fill Ivermectin
- www.ifm.org/find-a-practitioner (Functional Medicine)
- Post-COVID Care Centers (PCCC) by Survivor Corps






.png)

Comments
Post a Comment