The Role of Metabolic Health in Better COVID-19 Outcomes
Return guest Dr. Paul Saladino is a board-certified psychiatrist and also board certified in nutrition. He wrote "The Carnivore Code," which just came out in an updated second edition. In this interview, he discusses the impact metabolic health has on COVID-19 outcomes.
He's done a magnificent job explaining the science that supports the natural lifestyle strategies that optimize our immune systems to defeat not only COVID-19, but also most other infectious agents.I think that as we are faced with coronavirus, it's a reminder of the metabolic health and how critical that is. I think so much of the media focus right now is on the next drug or the coming vaccine … but all of those strategies kind of miss the point. [They're] just Band-Aids …
No drug is going to protect us from the next infection and the next infection. And one of the things that we're going to talk about today, which is so eerie, yet revealing, is all of this data suggesting that coronavirus susceptibility is intimately connected with metabolic health."
Immunometabolism Is an Important Field of Medicine
We've long known that metabolic health is crucial for robust immune function. Saladino believes immunometabolism — the connections between metabolism, metabolic health and the immune system — is easily one of the most important, if not the most important, field in emerging medicine.Saladino reviews NHANES data1 from 2009 to 2016, which reveal 87.8% of Americans are metabolically unhealthy, based on five parameters. That data is over four years old now, so the figure is clearly greater than 90% of the population today.
That means virtually everyone is at risk for Type 2 diabetes and all the chronic diseases associated with insulin resistance, which run the gamut from cancer to Alzheimer's.
"[NHANES] use criteria that we use to define metabolic syndrome," Saladino explains. "They use a waist circumference of less than 102 or 88 centimeters for men and women respectively, a fasting glucose of less than 100 milligrams per deciliter, hemoglobin A1c of less than 5.7, a systolic blood pressure less than 120, a diastolic blood pressure less than 80, and triglycerides less than 150, in addition to an HDL of greater than 40 for men and 50 for women, as criteria for metabolic health.What they found — and this is really the point that is so striking — is that only 12.2% of people met that criteria. That means 87.8% of people are metabolically unhealthy or have at least one of these metrics that suggests that they may have some degree of metabolic unhealth."
Similarly, data from the U.S. Centers for Disease Control and Prevention show that as of 2016, 39.8% of adults over the age of 20 were obese. When you include those who are overweight, that percentage skyrockets to 71%, and excess weight typically correlates with metabolic dysfunction and impaired health.
"Now, it's not so much an indictment on our population; it's an indication, it's a real call-to-arms to say, 'This is what we should be talking about,' and it's a real jumping-off point for discussions about how metabolic unhealth has repeatedly been connected with worse outcomes, [be it] COVID-19, MERS or seasonal flu. It's a huge piece of it, and I haven't really seen much media coverage of this at all."Insulin Resistance Is a Modern Plague
Indeed, while the media reports that the comorbidities include obesity, diabetes, age and being of color, they don't discuss the underlying problems, which are vitamin D deficiency and insulin resistance. As noted by Saladino:With aging, we see a direct correlation with insulin resistance. But the immune compromise, the insulin resistance that comes with aging, is not inevitable. It's an assumption, because 88% of the population are metabolically unhealthy.
The narrative here is very important because if we can escape the immunologic sort of dysfunction and insulin resistance that so often accompanies aging, then we can totally change our lifestyle."
Metabolic Age Is More Important Than Biological Age
Saladino discusses the results of a Nature Medicine study2 published in 2019, which looked at immune age and metabolic age using high-dimensional longitudinal monitoring:
"You can look at multiple measures of immunologic aging by looking at different varying proportions of immune cell subsets. This is all very esoteric and it looks complex, but the takeaway is that immune aging is associated with relative changes in different types of immune system response.What's very interesting is we see the same types of immune system response changes mirrored in people who have more severe coronavirus outcomes … One of the classic changes associated with insulin resistance, obesity and metabolic syndrome — these are all synonyms — is overactivation of the innate immune system, with decreasing activity in the adaptive immune system.
Characterized another way, we can look at the cytokines associated with different T-helper subsets. What we generally see … is that certain cytokines for T-helper 2 tend to predominate over T-helper 1, and you get changes in the way the innate and adaptive immune systems are responding to invaders. And that's what we see in people as they age.
That's associated with activation of different inflammasomes, like the NLRP3 inflammasome, which is associated with that innate immune system. The innate immune system is always activated; it's dendritic cells, macrophages, natural killer cells, neutrophils.
The adaptive immune system is T cells and B cells. So basically, what we see in immunologic compromise, what we see in insulin resistance, is that the innate immune system gets overactivated at the expense of the adaptive immune system.
You might say, 'Oh, that's good. One part of the immune system is more activated.' But what you have happening is that the adaptive immune system isn't able to be activated properly, and the resolution of the inflammation doesn't happen in the way it should."
So, the overarching principle is that it's not your biological age that matters so much, but rather it's your immune and metabolic age. The good news is those are more malleable than we are led to believe. From that perspective, we can address COVID-19 in completely different ways.
"What I want to empower people to understand is that this immunologic tolerance, this insulin resistance paradigm, has not been discussed at all despite the fact that there are tons of evidence that it's really, really important."
Cytokines
Cytokines are small proteins secreted by cells in your innate and adaptive immune systems. They serve to regulate diverse functions in your immune response. Cytokines are released by cells into your circulation or directly into your tissues.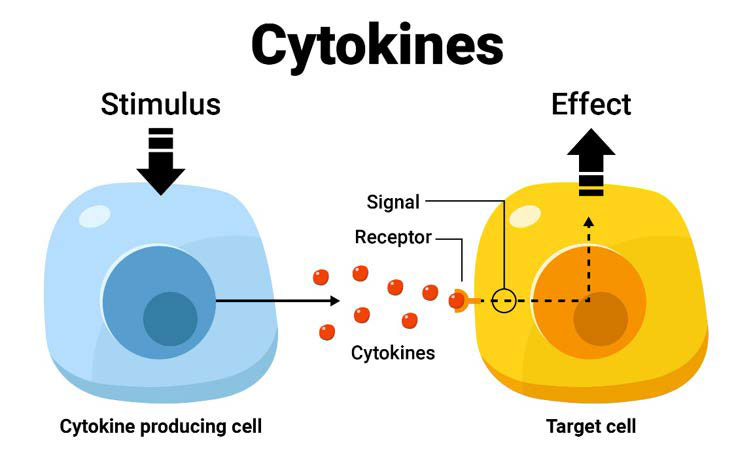
The cytokines locate target immune cells and interact with receptors on the target immune cells by binding to them. The interaction triggers or stimulates specific responses by the target cells.
In response to bacterial and viral infections such as COVID-19, your innate immune system generates both proinflammatory and anti-inflammatory cytokines.3 The inflammatory response plays a crucial role in the clinical manifestations of COVID-19. SARS-CoV-2 triggers an immune response against the virus, which, if uncontrolled, may result in lung damage, functional impairment, and reduced lung capacity.4,5,6,7
The SARS-CoV-2 viral infection-related inflammation and the subsequent cytokine storm in severe cases plays a crucial role in patient survival.8 The extensive and uncontrolled release of proinflammatory cytokines is termed the cytokine storm. Clinically, the cytokine storm commonly presents as systemic inflammation and multiple organ failure.9
Immunologic Tolerance Rises as Insulin Resistance Falls
One scientific article10 that speaks to this is "Association of Blood Glucose Control and Outcomes in Patients With COVID-19 and Pre-Existing Type 2 Diabetes," published in Cell Metabolism, June 2, 2020.
What it found was that when blood sugar is well-controlled and there's less glycemic variability, people do better when contracting COVID-19. When they have high levels of glycemic variability, which is indicative of insulin resistance, they fare much worse.
"So there's really no question at this point that glycemic variability, overall metabolic status, overall metabolic health are critical," Saladino says. The common mistake here is that you don't want to get that control back using drugs. Your best bet is to get it back using natural lifestyle strategies.
Another paper11 that demonstrates the impact of insulin resistance on COVID-19 was published in Cardiovascular Diabetology, May 11, 2020. It found you can use the triglyceride to glucose index (TyG index) as a gauge to predict the severity and mortality of COVID-19.
"Imagine that. There's an association of the insulin resistance marker, the TyG index — this is fasting triglycerides, fasting glucose — with the severity and mortality of COVID-19.This should be, in my opinion, mainstream news headlines, and the headlines should be, 'You can be stronger against coronavirus. You can have a stronger immune system. You can decrease your risk of having a severe coronavirus outcome.' But instead it's mostly fear, it's 'Hide in your homes. What's the next drug that's going to save us?' … Cardiovascular health is immune health. That is immunometabolism.
What you do to improve your heart health is also what you do to improve your immune health, is also what you do to improve your brain health, is also how you decrease your risk of Alzheimer's, is also how you decrease your risk of seasonal flu and every other single infectious illness that you will all encounter for the rest of your life. It's one thing; not 60 different drugs … which is why the [conventional] paradigm doesn't work."
Low LDL Associated With Greater COVID-19 Severity
Interestingly, Saladino cites research showing that low levels of LDL cholesterol are associated with greater COVID-19 severity. LDL and total cholesterol levels were significantly lower in COVID-19 patients as compared to healthy subjects. "To me, this is a really interesting [finding] in two ways," Saladino says, adding:When your body is doing an immunologic thing, when your body is fighting a pathogen, it totally makes sense that the LDL would be a part of that, in either LDLs consumed, or those who have lower LDL are more susceptible to infection.
This is something we see over and over, and there are even genetic syndromes of very low LDL, specifically one called Smith-Lemli-Opitz syndrome involving a genetic polymorphism in an enzyme that makes cholesterol.
People with that syndrome have very bad infections and they can be rescued by giving them egg yolks. So these people are given cholesterol in the form of egg yolks, or they're given supplemental cholesterol, and they do much better.
It's pretty clear that cholesterol, which is packaged into this LDL lipoprotein particle, is intimately involved in the immune response. And so, in someone who is metabolically healthy, a higher LDL above 100 or 150, or even 200 mg/dL might not be the horrible thing that we've all been taught it is, especially if the HDL, the triglycerides, the triglyceride to glucose index, that glycemic variability, are all pointing toward metabolic health …
It's about context. This LDL is a valuable immunologic particle and we can't just get myopic, looking at LDL. We have to think about it in terms of all these other measures."
Top Strategies to Improve Your Metabolic Health
Considering the fact that your metabolic health determines your COVID-19 risk, it would be a sound idea to implement strategies that will improve your metabolic flexibility and insulin sensitivity. Saladino's top recommendations for achieving that include:1.Eliminate processed carbohydrates, sugars, grains and vegetable oils — "I think that from a food perspective, those are the key evils that are really wreaking havoc on our metabolism," he says. The worst culprit of them all is probably vegetable oils. "Polyunsaturated vegetable oils are highly oxidizable and very metabolically damaging. So, start with them," Saladino says.
2.Eat animal foods — As noted in the paper,12 "Immune Function and Micronutrient Requirements Change Over the Life Course," published in the journal Nutrients, nutrient deficiencies that can compromise immune function include vitamins, A, C, D, E, B2, B6, B12, folate, iron, selenium and zinc.
These vitamins are primarily found in animal foods, which is why shunning animal foods tends to lead to nutrient deficiencies. Even folate is found in organ meats in highly bioavailable form. "If you want to have a robust immune system, you want to be metabolically healthy. You don't want to be insulin-resistant and you need to have nutrient adequacy in your diets," Saladino says.
"How do you get nutrient adequacy? You get these micronutrients from bioavailable sources in organ meats and in the muscle meat of animals." If you cannot stomach the idea of organ meats, consider using a desiccated organs supplement, such as those Saladino sells.13
3.Time-restricted eating — Compressing the window of time in which you eat down to six to eight hours a day, eating your last meal at least three hours before bedtime, is another very powerful strategy to improve your insulin sensitivity.
Eating a Varied, Real Food Diet Is Key
In short, eating real food, in a time-restricted window, is your surest bet to beat insulin resistance. Also remember to give some consideration to your macronutrient ratios.As explained by Saladino, while a low-fat, low-carb diet may reduce your insulin resistance, you're at high risk for nutrient deficiencies in the long term, as so many of the most bioavailable vitamins and minerals are found in animal-based fats.
Also include some of the healthiest carbohydrates, the nonprocessed carbohydrates, into your diet occasionally, and don't go either low-carb, high-fat all the time or low-fat, high-carb all the time. Having a mix, but having a robust amount of protein throughout … I think that's a sweet spot for most people."
Low Glutathione May Increase COVID-19 Severity
Saladino also cites a recent hypothesis highlighting the potential role of glutathione in COVID-19. The paper,14 "Endogenous Deficiency of Glutathione as the Most Likely Cause of Serious Manifestations of Death From Novel Coronavirus Infection (COVID-19): A Hypotheses Based on Literature Data and Own Observations," is written by a Russian medical doctor and Ph.D.
What he found was that the reactive-oxygen-species-to-glutathione ratio was able to predict the severity of COVID-19 and the patient's outcome. When the patient had a low ROS-to-glutathione ratio, the patient had a very mild case. The fever disappeared on the fourth day without any treatment whatsoever.
When the ROS-to-glutathione ratio was high, the patient developed air hunger on the fourth day, experienced significant fever, hoarseness, myalgia and fatigue persisting for 13 days. A patient with even higher ROS and lower reduced glutathione had critical disease requiring hospitalization for COVID-19-related pneumonia. According to the author:15
"Based on an exhaustive literature analysis and own observations, I proposed a hypothesis that glutathione deficiency is exactly the most plausible explanation for serious manifestation and death in COVID-19 infected patients.The major risk factors established for severe COVID-19 infection and relative glutathione deficiency found in COVID-19 infected patients with moderate-to-severe illness have converged me to two very important conclusions:
(1) oxidative stress contributes to hyper-inflammation of the lung leading to adverse disease outcomes such as acute respiratory distress syndrome, multiorgan failure and death;
(2) poor antioxidant defense due to endogenous glutathione deficiency as a result of decreased biosynthesis and/or increased depletion of GSH is the most probable cause of increased oxidative damage of the lung, regardless which of the factors aging, chronic disease comorbidity, smoking or some others were responsible for this deficit.
The hypothesis provides novel insights into the etiology and mechanisms responsible for serious manifestations of COVID-19 infection and justifies promising opportunities for effective treatment and prevention of the illness through glutathione recovering with N-acetylcysteine and reduced glutathione."
Glutathione, Zinc and Selenium
As noted by Saladino, these findings also tie into the issue of zinc and its importance for proper immune function, as zinc helps mitigate the oxidative stress reaction. The question is, why do these people have such low glutathione in the first place?
Saladino believes it's probably due to underlying nutritional deficiencies such as glycine deficiency, or oxidative stress caused by smoking, heavy metal toxicity, EMF exposure, eating lots of processed vegetable oils or insulin resistance. Any of these could cause low glutathione.
To improve your glutathione, you need zinc, and zinc in combination with hydroxychloroquine (a zinc ionophore or zinc transporter) has been shown effective in the treatment of COVID-19.
N-acetyl cysteine (NAC), meanwhile, is a precursor of glutathione, and may protect against coagulation problems associated with COVID-19, as it counteracts hypercoagulation and breaks down blood clots.
Selenium is also important, as some of the enzymes involved in glutathione production are selenium-dependent. Saladino cites research showing an association between regional selenium status and the severity of COVID-19 outcome cases in China. The lower the amount of selenium in the hair, the lower the cure rate was.
"Why is this? It's probably because glutathione peroxidase and thioredoxin reductase are selenium- dependent enzymes, and these enzymes are intimately connected by controlling this antioxidant redox system," Saladino explains."So, what we're seeing is this huge immunologic injury, this imbalance of the innate and adaptive immune system, we're seeing insulin resistance, and we're seeing diffused oxidative damage, and all that stuff can probably be controlled with lifestyle. That's the huge takeaway."
One of the best ways to increase glutathione, though, is molecular hydrogen. It is my absolute favorite as it does so selectively and will not increase glutathione unnecessarily if you don't need it.
More Information
We cover a lot of ground in this interview, far more than has been summarized here, so for more details, be sure to listen to the interview. Saladino is a wellspring of well-researched information. We also review:
- The use of quercetin in lieu of hydroxychloroquine, either of which needs to be taken with zinc, at the first signs of symptoms.
- The hazards of oxalates, found in many plant foods and the benefits of a carnivore diet.
- Links between COVID-19 and pulmonary vasculitis — A new hypothesis suggests SARS-CoV-2 attacks the endothelial cells that line the blood vessels surrounding the lungs' air sacs, or alveoli, causing fluid leakage and blood clots. According to Saladino, low glutathione may be at play here as well.
- How you can improve your insulin sensitivity in as little as nine days by eliminating all fructose.
To learn more, be sure to visit his website, CarnivoreMD.com, and pick up a copy of "The Carnivore Code," now in its updated second edition. He also has a great podcast called "Fundamental Health." On the social media platforms, you can find him by searching for @carnivoreMD.
"If those who are susceptible to COVID-19 due to insulin resistance and diabetes are able to use this as a wake-up call and change their metabolic health, they will change the quality of life for the entire time that they're living," Saladino says."My dad is a perfect example of this. He's 70 years old, a retired internist, and I'm going to get him a continuous glucose monitor. He's not as metabolically healthy as he should be, but I'm encouraging him to improve his metabolic health.
And the beauty of that might just be that if coronavirus is the impetus, if coronavirus is the trigger that he needs to change his metabolic health — to use a continuous glucose monitor, to show himself his glycemic variability and understand how much risk that puts him at, or just to give him an indication that he's a little insulin-resistant because he's eating bread or vegetable oil, or not getting enough nutrients.
If he makes the change, he's decreasing his risk of coronavirus, but he's also decreasing his risk of seasonal flu, diabetic complications, coronary artery disease, hypertension and stroke. I mean, the list goes on and on. That's what you and I are about, and that's what I think it's all focused on."
- 1 Metabolic Syndrome and Related Disorders February 8, 2019 DOI: 10.1089/met.2018.0105
- 2 Nature Medicine March 6, 2020; 25: 487–495
- 3 Lancet 2020 Feb 15;395(10223):497-506
- 4 J. Med. Virol. 2020; 92: 424–432
- 5 Autoimmun. Rev. 2020; 19(6): 102537
- 6 Ann. Hematol. 2020; 99: 1205-1208
- 7, 9 Lancet 2020 Mar 28;395(10229):1033-1034
- 8 Clin. Immunol. 2020 May;214:108393
- 10 Cell Metabolism June 2, 2020; 31(6): 1068-1077.e3
- 11 Cardiovascular Diabetology May 11, 2020; 19 article number 58
- 12 Nutrients 2018 Oct 17;10(10):1531
- 13 HeartAndSoilSupplements.com
- 14, 15 Researchgate.net April 2020
Original Article: https://articles.mercola.com/sites/articles/archive/2022/01/02/metabolic-health-impact-on-covid-19-severity.aspx
Additional and Updated Evidence
Diet
- The Perez-Araluce study refers to a Mediterranean diet.
- The Vietnamese Nguyen study refers to a 'healthy diet' that is defined by a higher intake frequency of fruits and vegetables, whole grains, dairy and fish.
- The Iranian Moludi study refers to a 'high inflammatory' diet as a risk factor to a more severe COVID-19.
- The Merino study of more than 500,000 participants in UK and USA showed lower risk or COVID-19 cases and severity for higher healthful plant-based diet scores.
- The Kim study in 6 countries also showed plant-based diets were associated with lower odds of moderate-to-severe COVID-19.
Exercise
Most studies analyze exercise/physical activity levels before infection, comparing regular/moderate exercise and lower/no exercise. Risk may increase with more extreme activity levels.






.png)

Comments
Post a Comment