10 Natural Treatments for Long COVID (2025)
Federal data published by the US CDC in 2024 found that 17.9% (National Estimate) of adults who previously had a COVID-19 infection are currently experiencing symptoms of long COVID. Females tend to have a relatively higher risk as compared to males.
If you’re still coping with symptoms three months or more after being infected with COVID-19, you’re considered a COVID long-hauler. As we learn more about post-COVID syndrome, however, the definition has been refined to be more accurate and useful:
- Subacute or ongoing COVID-19 (post-acute COVID-19 syndrome): symptoms continuing beyond four weeks from acute infection, up to 12 weeks.
- Post-acute sequelae of COVID-19 (PASC): symptoms persisting beyond the four weeks after acute infection.
- Post-COVID-19 syndrome (long COVID, long-hauler’s syndrome): chronic ongoing COVID-19 symptoms beyond 12 weeks from acute infection.
With 200-plus symptoms linked to long COVID, treatment starts by pinpointing specific medical conditions and referring patients to the right clinicians. These might be lung specialists, heart specialists or brain rehabilitation experts. Patients need a carefully designed but flexible long haul COVID treatment protocol tailored to their particular symptoms and needs.
Updates:
In this Article:
- Long Haulers Symptoms
- Natural Treatments
- Nattokinase
- Vitamin D
- Probiotics
- Melatonin
- Vitamin C
- Omega-3 fatty acids
- N-Acetyl-L-Cysteine (NAC)
- Quercetin, EGCG and Curcumin
- Zinc
- Resveratrol
- FLCCC I-Recover Protocol
Long Haulers Symptoms
While the CDC tracks the prevalence of 26 common post-COVID conditions affecting a significant body system, more than 50 long-term effects, particularly fatigue, headache, attention disorders, shortness of breath and hair shedding, are now attributed to long-hauler’s syndrome (R).
The global prevalence of post-COVID syndrome four months after the infection is now estimated at 49% of all patients (Journal of Infectious Diseases, November 2022). About 54% of hospitalized patients had long-hauler symptoms and about 34% of non-hospitalized patients had symptoms. This is a very important point to note i.e. a severe disease tend to lead to long COVID as opposed to a mild disease.
Among those who were hospitalized, only 26% fully recovered after five months (R), and nearly half still had symptoms one year later (R). Those who needed mechanical ventilation were 58% less likely to heal fully; obese people were half as likely to recover fully (R). At the two-year mark, 55% of hospitalized patients had at least one COVID-19 symptom, compared to 68% six months after infection. Patients generally had poorer health two years later and still experienced pain, fatigue, problems with sleeping and mental health issues. They went to a doctor more often, had ongoing difficulty exercising, and experienced poor quality of life (R).
Although numerous reports describe the epidemiology and clinical features of
post-COVID syndrome, studies evaluating treatment options are glaringly
sparse. In general, while ‘Long COVID treatment”
should be individualized, the following supplements may have a role in the
treatment of this disorder.
Natural Treatments for Long Haulers
We will cover some of the best natural supplements below, that may have a
role in the treatment of this disorder. Please take note that the purpose of
this article is to educate and to assist you in doing your own research.
Before you take any supplements, it's best you find a doctor to discuss with.
1. Nattokinase, Lumbrokinase and Serrapeptase
If you’ve had COVID-19, especially if it was a severe case, be aware that blood clots and heart problems, including heart attack, can occur for 90 days or more. It’s believed that remnants of the virus remain in the nervous system, the lungs, the heart and other organs.If the symptoms include major shortness of breath, cough with blood in it or pain on one side when you take a deep breath, it could be due to a late pulmonary embolism or a blood clot going to the lungs.
Nattokinase (NK) is an enzyme derived from a traditional Japanese food called natto, and it is thought to help lower cholesterol, reduce inflammation, and improve circulation.
Furthermore, a study has also suggests that daily NK supplementation is an effective way to manage the progression of atherosclerosis and potentially may be a better alternative to statins which are commonly used to reduce atherosclerosis and further to prevent cardiovascular attack and stroke in patients.
Authors found that NK at a dose of 10,800 FU/day effectively managed the progression of atherosclerosis and hyperlipidemia with a significant improvement in the lipid profile. The lipid-lowering effect of NK was more prominent in subjects who smoked, drank alcohol, and subjects with higher BMI. Regular exercise further improved the effects of NK.
Co-administration of vitamin K2 and aspirin with NK produced a synergetic effect. In conclusion, the data demonstrate that atherosclerosis progression and hyperlipidemia can be effectively managed with NK at a dose of 10,800 FU/day. The lower dose of 3,600 FU per day is ineffective. Some lifestyle factors and the coadministration of vitamin K2 and aspirin lead to improved outcomes in the use of NK. The findings provide clinical evidence on the effective dose of NK in the management of cardiovascular disease and challenge the recommended dose of 2,000 FU per day.
Tanikawa et al. (2022) examined the effect of nattokinase on the COVID-19 spike protein. In the first experiment, they demonstrated that spike was degraded in a time and dose-dependent manner in a cell lysate preparation that could be similar to a vaccine recipient. The second experiment demonstrated that nattokinase degraded the spike protein in SARS-CoV-2 infected cells. This was reproduced in a similar study done by Oba and colleagues in 2021.
Lumbrokinase and Serrapeptase (Alternatives)
Lumbrokinase and serrapeptase are alternatives to nattokinase. You can alternate between these enzymes — one day take nattokinase and the next take lumbrokinase or serrapeptase — because you’ll need to be on it for about three months and you can develop a sensitivity to them over time.
Anyone who had COVID-19, especially with significant symptoms, should consider taking digestive fibrinolytic enzymes to be sure you don’t have any clotting. An alternative to determine if clotting is occurring is a test called D-dimer, although it can be pricey. D-dimer is a protein fragment produced by the body when a blood clot dissolves.
It’s typically undetectable or present only at very low levels, buts its level may significantly rise when the body is forming and breaking down blood clots (R). If your d-dimer test is low, then you don’t need to take the enzymes. Likewise, if you had a very mild, cold-like case, of COVID-19, you probably don’t need them.
Anyone who had COVID-19, especially with significant symptoms, should consider taking digestive fibrinolytic enzymes to be sure you don’t have any clotting. An alternative to determine if clotting is occurring is a test called D-dimer, although it can be pricey. D-dimer is a protein fragment produced by the body when a blood clot dissolves.
It’s typically undetectable or present only at very low levels, buts its level may significantly rise when the body is forming and breaking down blood clots (R). If your d-dimer test is low, then you don’t need to take the enzymes. Likewise, if you had a very mild, cold-like case, of COVID-19, you probably don’t need them.
2. Melatonin
Melatonin has anti-inflammatory and antioxidant properties and is a
powerful regulator of mitochondrial function [R]. It also supports the gut lining, which promotes healthy immune
function.
Supplementing with 1 - 2 mg of melatonin at bedtime might benefit those whose sleep–wake cycles have become dysregulated with long COVID.
Supplementing with 1 - 2 mg of melatonin at bedtime might benefit those whose sleep–wake cycles have become dysregulated with long COVID.
3. Probiotics
COVID can wreak havoc on the gut microbiome, but research on specific probiotic strains that can best restore balance following the syndrome’s particular damage is in its infancy. Leo Galland, MD, a functional-medicine internist in New York City, is looking into soil-derived bacteria of the genus Bacillus because it may have natural antibiotic properties, though there’s not yet enough data to make specific recommendations.One Swedish study demonstrated that taking probiotics for 14 days could help alleviate some of the symptoms of long COVID, namely muscle soreness and brain fog. We also recommend optimizing your gut microbiome by avoiding processed vegetable oils, processed foods and conventionally raised meats in animal products.
Probiotics is one of the first line therapies of the FLCCC i-Recover protocol for post-vaccine syndrome.
Eating fermented foods, such as sauerkraut, yogurt, kefir, and kimchi, can help fortify and support the gut’s microbiome. And in the event of ongoing gut disturbances, working with a functional-medicine provider to design a well-rounded prebiotic and probiotic protocol can help bring the microbiome back into balance.
As reported in this short news clip, research evidence shows that probiotics may help reduce long-haul symptoms after COVID-19. Some people experience symptoms for weeks or months after a COVID-19 infection has resolved. When these symptoms persist for four weeks or more, they are known as long COVID, long-haul COVID, chronic COVID or long-haul syndrome.
4. Vitamin D
Vitamin D3 is essential for supporting healthy immune system function. It works hand in hand with your body to modulate both innate and adaptive immune responses which regulate everything from reactivity to antigens and pathogens.Maintaining good vitamin D status should be a priority even as a preventive measure, and may help restrain inflammation from elevating during COVID in the first place.
The majority of those with post-COVID-19 syndrome continue to have low levels of vitamin D in their bodies.
Vitamin D is also one of the recommended treatments in FLCCC's i-Recover protocol for post-vaccine syndrome.
According to FLCCC's i-Recover protocol for Long COVID, the majority of those with post-COVID-19 syndrome continue to have hypovitaminosis D (low vitamin D level). See tables 1 or 2 for vitamin D supplementation below.

5. Vitamin C
Vitamin C has important anti-inflammatory, antioxidant, and immune-enhancing properties, including increased synthesis of type I interferons. [R] Avoid in patients with a history of kidney stones. Oral Vitamin C also helps promote growth of protective bacterial populations in the microbiome.
Vitamin C inhibits histamine. Healthcare professionals are administering vitamin C intravenously to deliver it directly into their patient’s bloodstream to be immediately available. Liposomal vitamin C is the next best option. It’s the most bioavailable form of vitamin C on the market today. The liposomal form can survive the digestive process to be up to 135% better than traditional oral vitamin C.
Long-COVID patients can supplement with liposomal vitamin C 500 mg twice a day.
Related: Best Vitamin C Supplement
6. Omega-3 fatty acids
Vascepa, Lovaza or DHA/EPA 4 g day. Omega-3 fatty acids play an
important role in the resolution of inflammation by inducing
resolvin production. [Ref, Ref]
Omega-3 is also part of the first line treatments of the FLCCC
i-Recover protocol (below).
7. Quercetin, EGCG and Curcumin
Quercetin has broad spectrum anti-inflammatory properties. These
natural flavonoids inhibit mast cells and have been demonstrated
to reduce neuro-inflammation.
Flavonoids have broad spectrum anti-inflammatory properties,
inhibit mast cells, [R] and have been demonstrated to reduce neuroinflammation. [R] Due to the possible drug interaction between quercetin and
ivermectin (see below) these drugs should not be taken
simultaneously (i.e., should be staggered morning and
night).
Quercetin appears to bind to the spike protein of the coronavirus, inhibit inflammatory pathways, and block replication of infected cells. It is also antiviral and completely safe. In addition to getting sources of quercetin from diet, long-COVID patients can supplement with 250 - 500 mg a day.
Other phytonutrients such as EGCG (epigallocatechin gallate, a
polyphenol found in green tea) and curcumin (found in turmeric)
can also decrease inflammation and rebalance the immune
system.
8. N-Acetyl-L-Cysteine (NAC)
NAC is an amino acid that the body uses to create glutathione, the body’s master detoxifier. Glutathione is your master detoxifier and the most powerful free radical scavenger produced by your body.Eating plenty of cruciferous vegetables (such as kale, broccoli, and cabbage), as well as avocado, okra, spinach, and alliums, can help bolster levels of glutathione, as can supplementing with NAC.
A 2017 paper found NAC has potent thrombolytic effects, meaning it
breaks down blood clots once they've formed.
Importantly, NAC may also protect against other problems
associated with COVID-19, including the hypercoagulation that
can result in stroke and/or blood clots that impair the ability to exchange oxygen in the
lungs.
Many COVID-19 patients experience serious blood clots, and NAC counteracts hypercoagulation, as it has both anticoagulant and platelet-inhibiting properties.
Many COVID-19 patients experience serious blood clots, and NAC counteracts hypercoagulation, as it has both anticoagulant and platelet-inhibiting properties.
Aaron Hartman, MD, founder of the Richmond Integrative and Functional Medicine clinic in Richmond, Va., describes one patient, a 26-year-old woman, whose symptoms — persistent low oxygen and shortness of breath — following a bout of COVID resolved after treatment that included NAC as well as omega-3 fish oil.
“NAC is one of the more important nutrients for people who get shortness of breath with COVID, because of its ability to break down those really, really small blood clots called micro-emboli,” explains Hartman.
9. Zinc
Zinc is essential for healthy immune function. A 2020 review published in the International Journal of Infectious Diseases has found that zinc deficiency can increase the risk of poor outcomes in viral infections, including COVID-19.Foods that are rich in zinc include meat, poultry, shellfish, eggs, dairy, seeds, nuts, legumes, sweet potatoes, quinoa, and green leafy vegetables.
10. Resveratrol
Resveratrol is a polyphenol with antioxidant and anti-inflammatory effects that’s found in red grapes, red wine, peanuts, and some berries. It’s also available as a supplement.
Leo Galland, MD, a functional-medicine internist in New York City, has found it to be particularly helpful in restoring his COVID patients to health. “Resveratrol has a number of beneficial effects on coronavirus infection,” he notes. “It supports ACE-2 function, it inhibits the growth of the deadly MERS coronavirus through multiple mechanisms, and it diminishes the kind of inflammation associated with coronavirus infection.”
Galland treated a physician in her 60s who’d been sick with COVID for six weeks, continuing to run daily fevers with brain fog and fatigue. He prescribed a combination of herbs and supplements, including resveratrol, and her symptoms resolved within a couple of weeks.
He recommends long-COVID patients supplement with 200 mg of resveratrol twice a day.
He recommends long-COVID patients supplement with 200 mg of resveratrol twice a day.
FLCCC I-Recover Protocol
Due to the marked overlap between long COVID and post-vaccine syndrome, please refer to the I-RECOVER Post-Vaccine Treatment protocol below for detailed treatment strategies.
The I-Recover protocol has been updated and below is their latest version, based on the FLCCC document called “An Approach to Managing Post-Vaccine Syndrome” (March 2024).
The I-Recover protocol has been updated and below is their latest version, based on the FLCCC document called “An Approach to Managing Post-Vaccine Syndrome” (March 2024).
Though there are many long haulers treatment protocols out there, we consider and recommend the I-Recover protocol as one of the best.
Given the lack of clinical trials of long-haul COVID-19 syndrome, these recommendations are based on the abnormal changes within the body associated with the COVID-19 disease and post viral illnesses along with the collective experience of FLCCC members.
This protocol has also been used to treat post-vaccine inflammatory syndromes with similar success. As with all FLCCC Alliance protocols, the components, doses, and durations will evolve as more clinical data accumulates.
Due to the marked overlap between long COVID and post-vaccine syndrome, please refer to the I-RECOVER Post-Vaccine Treatment protocol below for detailed treatment strategies.
Note that there are two post-vaccine protocols, one to treat post vaccine injury (I-Recover Post Vaccine) and the other to prevent post vaccine injury (I-Prevent Post Vaccine).
Treatment must be individualized according to each patient’s presenting symptoms and disease syndromes. It is likely that not all patients will respond equally to the same intervention; a particular intervention may be life-saving for one patient and totally ineffective for another. Early treatment is essential; it is likely that the response to treatment will be attenuated when treatment is delayed.
Patients with post-vaccine syndrome should do whatever they can to prevent themselves from getting COVID-19. This may include a preventative protocol (see I-PREVENT) or early treatment in the event you do contract the virus or suspect infection (see I-CARE). COVID-19 will likely exacerbate the symptoms of vaccine injury.
Once a patient has shown improvement, the various interventions should be reduced or stopped one at a time. A less intensive maintenance approach is then suggested.
The core problem in post-vaccine syndrome is long-lasting “immune dysregulation.” The most important treatment goal is to help the body restore a healthy immune system — in other words, to let the body heal itself. Our recommended treatment strategy involves two major approaches:- Promote autophagy to help rid the cells of the spike protein
- Use interventions that limit the toxicity/pathogenicity of the spike protein
FLCCC recommend the use of immune-modulating agents and interventions to dampen and normalize the immune system rather than the use of immunosuppressant drugs, which may make the condition worse.
Though there are many long haulers treatment protocols out there, we consider and recommend the I-Recover protocol as one of the best.
Given the lack of clinical trials of long-haul COVID-19 syndrome, these recommendations are based on the abnormal changes within the body associated with the COVID-19 disease and post viral illnesses along with the collective experience of FLCCC members.
This protocol has also been used to treat post-vaccine inflammatory syndromes with similar success. As with all FLCCC Alliance protocols, the components, doses, and durations will evolve as more clinical data accumulates.
Note that there are two post-vaccine protocols, one to treat post vaccine injury (I-Recover Post Vaccine) and the other to prevent post vaccine injury (I-Prevent Post Vaccine).
Patients with post-vaccine syndrome should do whatever they can to prevent themselves from getting COVID-19. This may include a preventative protocol (see I-PREVENT) or early treatment in the event you do contract the virus or suspect infection (see I-CARE). COVID-19 will likely exacerbate the symptoms of vaccine injury.
Once a patient has shown improvement, the various interventions should be reduced or stopped one at a time. A less intensive maintenance approach is then suggested.
The core problem in post-vaccine syndrome is long-lasting “immune dysregulation.” The most important treatment goal is to help the body restore a healthy immune system — in other words, to let the body heal itself. Our recommended treatment strategy involves two major approaches:
Treatment must be individualized according to each patient’s presenting symptoms and disease syndromes. It is likely that not all patients will respond equally to the same intervention; a particular intervention may be life-saving for one patient and totally ineffective for another. Early treatment is essential; it is likely that the response to treatment will be attenuated when treatment is delayed.
Patients with post-vaccine syndrome should do whatever they can to prevent themselves from getting COVID-19. This may include a preventative protocol (see I-PREVENT) or early treatment in the event you do contract the virus or suspect infection (see I-CARE). COVID-19 will likely exacerbate the symptoms of vaccine injury.
Once a patient has shown improvement, the various interventions should be reduced or stopped one at a time. A less intensive maintenance approach is then suggested.
The core problem in post-vaccine syndrome is long-lasting “immune dysregulation.” The most important treatment goal is to help the body restore a healthy immune system — in other words, to let the body heal itself. Our recommended treatment strategy involves two major approaches:
- Promote autophagy to help rid the cells of the spike protein
- Use interventions that limit the toxicity/pathogenicity of the spike protein
First Line Therapies
(Not symptom specific; listed in order of importance)- Intermittent daily fasting or periodic daily fasts. (Read more)
- Nattokinase (Tanikawa 2022, McCullough 2023): 100-200 mg (2000- 4000 Fibrinolytic Units) twice daily.
- Ivermectin : 0.2 - 0.3 mg/kg daily. (Stone 2022) (Find Provider)
- Moderating physical activity
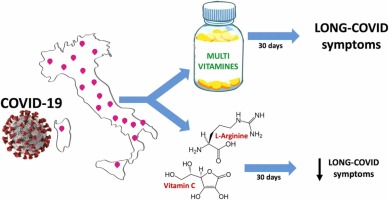
- L-Arginine (1.5 -2g twice daily) and Vitamin C (1000 mg orally two to three times daily)*
- Low-dose naltrexone: 1- 4.5 mg daily
- Treatment of Mast Cell Activation
- Sunlight and Photobiomodulation (Red Light Therapy)
- Melatonin: 2-6 mg slow release/extended release prior to bedtime
- Bromelain + NAC (Amazon)
- Nigella sativa (Black Seed Oil)
- Resveratrol or a combination flavonoid
- Probiotics/Prebiotics (Lau 2023)
- Vagus Nerve Stimulation and nicotinic agonists
- Metformin
*Liposomal Vitamin C (Amazon) or whole food vitamin C (PaleoValley Essential C Complex): 1000 mg orally two to three times a day.
(Not symptom specific; listed in order of importance)
- Intermittent daily fasting or periodic daily fasts. (Read more)
- Nattokinase (Tanikawa 2022, McCullough 2023): 100-200 mg (2000- 4000 Fibrinolytic Units) twice daily.
- Ivermectin : 0.2 - 0.3 mg/kg daily. (Stone 2022) (Find Provider)
- Moderating physical activity
- L-Arginine (1.5 -2g twice daily) and Vitamin C (1000 mg orally two to three times daily)*
- Low-dose naltrexone: 1- 4.5 mg daily
- Treatment of Mast Cell Activation
- Sunlight and Photobiomodulation (Red Light Therapy)
- Melatonin: 2-6 mg slow release/extended release prior to bedtime
- Bromelain + NAC (Amazon)
- Nigella sativa (Black Seed Oil)
- Resveratrol or a combination flavonoid
- Probiotics/Prebiotics (Lau 2023)
- Vagus Nerve Stimulation and nicotinic agonists
- Metformin
*Liposomal Vitamin C (Amazon) or whole food vitamin C (PaleoValley Essential C Complex): 1000 mg orally two to three times a day.
Second-Line Therapies
(Listed in order of importance)- Vitamin D3 (4000-5000 units/day) and Vitamin K2 (100 mcg/day).
- N-acetyl cysteine (NAC) (ZeroSpike Project): 600-1500 mg/day
- Cardio Miracle™ and L-arginine/L-citrulline supplements
- Omega-3 fatty acids: FLCCC suggest a combination of EPA/DHA with an initial dose of 1 g/day (combined EPA and DHA) and increasing up to 4 g/day (of the active omega-3 fatty acids).
- Triple anticoagulation
- Magnesium
- Sildenafil (with or without L-arginine and L-citrulline)
- Spermidine
- Non-invasive brain stimulation
- Intravenous Vitamin C: 25 g weekly, together with oral Vitamin C 1000 mg (1 gram) 2-3 times per day. (Find Provider)
- Behavioral modification, relaxation therapy, mindfulness therapy, and psychological support
(Listed in order of importance)
- Vitamin D3 (4000-5000 units/day) and Vitamin K2 (100 mcg/day).
- N-acetyl cysteine (NAC) (ZeroSpike Project): 600-1500 mg/day
- Cardio Miracle™ and L-arginine/L-citrulline supplements
- Omega-3 fatty acids: FLCCC suggest a combination of EPA/DHA with an initial dose of 1 g/day (combined EPA and DHA) and increasing up to 4 g/day (of the active omega-3 fatty acids).
- Triple anticoagulation
- Magnesium
- Sildenafil (with or without L-arginine and L-citrulline)
- Spermidine
- Non-invasive brain stimulation
- Intravenous Vitamin C: 25 g weekly, together with oral Vitamin C 1000 mg (1 gram) 2-3 times per day. (Find Provider)
- Behavioral modification, relaxation therapy, mindfulness therapy, and psychological support
Third Line Therapies
- Hyperbaric oxygen therapy (HBOT)
- Low Magnitude Mechanical Stimulation
- “Mitochondrial energy optimizer” with pyrroloquinoline quinone, glycophospholipids, CoQ10, NADH, and other nutrients (e.g., Life Extension Energy Optimizer, Restorative Solutions Mitochondrial Nutrition PQQ, Researched Nutritionals ATP 360® and ATP Fuel® and PureEncapsulations Mitochondria-ATP)
- Low-dose corticosteroid
Warning (anaesthesia and surgery):
Patients should notify their anesthesia team if using the following medications and/or nutraceuticals, as they can increase the risk of Serotonin syndrome (SS) with opioid administration:- Methylene blue
- Curcumin
- Nigella Sativa
- Selective Serotonin Reuptake Inhibitors (SSRIs)
Note: There are also some important cautions and contraindications that should be carefully reviewed within the more comprehensive and detailed document called “An Approach to Managing Post-Vaccine Syndrome” (March 2024) and which should be discussed with a qualified provider as well.
It appears that vaccine-injured patients can be grouped into two categories: i) ivermectin responders and ii) ivermectin non-responders. This distinction is important, as the latter are more difficult to treat and require more aggressive therapy.
- Hyperbaric oxygen therapy (HBOT)
- Low Magnitude Mechanical Stimulation
- “Mitochondrial energy optimizer” with pyrroloquinoline quinone, glycophospholipids, CoQ10, NADH, and other nutrients (e.g., Life Extension Energy Optimizer, Restorative Solutions Mitochondrial Nutrition PQQ, Researched Nutritionals ATP 360® and ATP Fuel® and PureEncapsulations Mitochondria-ATP)
- Low-dose corticosteroid
Warning (anaesthesia and surgery):
Patients should notify their anesthesia team if using the following medications and/or nutraceuticals, as they can increase the risk of Serotonin syndrome (SS) with opioid administration:
- Methylene blue
- Curcumin
- Nigella Sativa
- Selective Serotonin Reuptake Inhibitors (SSRIs)
Note: There are also some important cautions and contraindications that should be carefully reviewed within the more comprehensive and detailed document called “An Approach to Managing Post-Vaccine Syndrome” (March 2024) and which should be discussed with a qualified provider as well.
It appears that vaccine-injured patients can be grouped into two categories: i) ivermectin responders and ii) ivermectin non-responders. This distinction is important, as the latter are more difficult to treat and require more aggressive therapy.
For ivermectin responders, prolonged and chronic daily treatment is often necessary to support their recovery. In many, if the daily ivermectin is discontinued worsening symptoms often recur within days.
Ivermectin is best taken with or just following a meal, for greater absorption.
For ivermectin responders, prolonged and chronic daily treatment is often necessary to support their recovery. In many, if the daily ivermectin is discontinued worsening symptoms often recur within days.
Ivermectin is best taken with or just following a meal, for greater absorption.
Related:
- Find health care providers: FIND A DOCTOR WHO WILL PRESCRIBE IVERMECTIN, HYDROXYCHLOROQUINE AND EARLY OUTPATIENT TREATMENTS FOR COVID-19 (USA)
- The first ever spike detox protocol appeared in the US Medical Literature and now it is available to you!
- This base spike protein detox protocol consists of these three powerful ingredients: Spike Support's Nattokinase, Bromelain, and Tumeric Extract.
- 4x More Nattokinase Than Original Spike Support.
- Vaccinated or not, prioritizing your well-being has never been more crucial.
- Buy this ultimate detox bundle today, researched by Dr. Peter McCullough.
- Recommended to maintain daily health for anyone exposed to COVID, vaccines, or shedding – and may help your body repair itself and remain at optimal health.
Where to buy Ultimate Spike Detox: Available on The Wellness Company's website. Here is the link: Base Spike Detox Trio.


.png)
.png)






.png)

Comments
Post a Comment