Should You Test For Spike Protein?
Given the current spotlight on the spike protein, it’s no wonder it’s on everyone’s mind:
- Increased Awareness: With the wealth of new studies and discussions, public awareness about the spike protein’s role has surged.
- Shedding Phenomenon: Recent insights into how the spike protein can be shared among individuals have heightened concerns.
Can You Test For Spike Proteins?
- There is no test for the spike protein, only “spike protein antibodies”.
Instead, tests commonly look for antibodies against the spike protein of the SARS-CoV-2 virus. These antibodies are part of the body’s immune response to the presence of the spike protein (be it from a COVID infection or the COVID shot). So, the tests are looking for antibodies to SARS-CoV-2, which means they could be used to “infer” previous exposure to the spike. The idea that some practitioners have is that a higher antibody response could mean a higher level of floating spike in the blood.
Should You Test for Your Spike Antibody Level?
Maybe a better question to ask is, “Should you test for your spike antibody?”
With all the talk about the spike, it’s natural to want to test yourself. Even if you aren’t sick, that creeping “what if?” feeling is hard to ignore.And, you might be surprised to hear there are more strong arguments against the need for COVID-19 antibody testing:
- Healthcare Should Aim to Control Costs
- Before COVID, Testing for Viral Particles Was Rarely Standard Practice
- Many Spike Protein Treatments Have Other Health Benefits
- Immune System Response Varies Widely Among Individuals
- Focus on Overall Health and Prevention
1. Healthcare Should Aim to Control Costs
In healthcare, the aim is always to provide the best possible care at the best possible price. But let’s be honest, our current healthcare system has strayed from this path quite a bit. That’s a big issue on its own.
Even so, keeping healthcare costs low is something we must strive for. Lab tests, in general, are expensive—and that is no different for the spike protein antibody test. Tests are especially expensive for people without insurance. Since a spike antibody test often won’t drive patient care, it may not be as important to overall health outcomes.
A provider tailors patient care per patient and based on the patient’s needs. Often, care is directed based on response to treatment intervention and not on testing alone. This principle should guide us in considering spike protein antibody testing. If you’re showing symptoms associated with spike protein, the focus should be on addressing those symptoms directly, rather than fixating on test results.
After all, a positive test result won’t necessarily alter the course of your treatment. Why incur the additional expense? Prioritizing symptom management ensures that resources are used where they can make a real difference in patient care.
2. Before COVID, Testing for Viral Particles Was Rarely Standard Practice
Unless you were living on another planet, you must remember that before COVID, the impulse to test ourselves endlessly was far less elevated. Maybe that’s because tests were not being forced upon us at every possible opportunity like they were from 2020 to mid-2023.
The surge in testing frequency we saw during COVID didn’t equate to improved health outcomes. Though the spike antibody test provides another data point, the treatment of symptoms will likely remain the same despite what the test results show.
3. Many Spike Protein Treatments Have Other Health Benefits
One reason you’d want to know about your antibody results? To decide whether or not to start addressing the spike protein in your body.
It makes sense: why would you treat something if it isn’t there? Well, do you have symptoms? If so, treatment could help. If you don’t have symptoms, don’t worry!
Having said all that, OTC supplements like Nattokinase, Lumbrokinase, and Nigella Sativa are beneficial to health for many reasons, not just for long COVID and long Vax!
👉 Learn more: OTC Long Vax Treatments
4. Immune System Response Varies Widely Among Individuals
We are all human, but our immune systems vary widely. As a result, so do our immune responses.
That could mean that some people have a robust immune response to very little spike protein. And it could mean that some people have a modest response to a large amount of spike.
Adding to the complexity, spike antibodies alone cannot remove the spike protein from the body. Our understanding of how spike antibodies interact with the overall immune response and other processes involved in eliminating spike from our cells is still evolving.
In other words, it’s possible that a negative result and a positive result could both be telling you nothing about the actual level of spike protein in your body.
5. Focus on Overall Health and Prevention
The key to navigating health today isn’t just about testing for specific proteins or antibodies; it’s about overall well-being. Simple steps like eating right, having a healthy movement routine, and managing stress are foundational.
Let’s strive to keep your immune system strong and reduce the need for medical interventions! Remember, good health practices are our best bet for a resilient body and a manageable healthcare system.👉 Learn more: FLCCC Eat Well Guide to Healthy Eating
Dr. Peter McCullough’s X Post (2025)
Base Spike Detox Protocol Success Story
Dr. McCullough : I am a physician who got Pfizer 2020, 2021 and 2021 to keep working at hospital in Colorado. I am happy to report: MARCH 2024 Spike ABY 1:25,000. Using the McCullough protocol now six months, my Spike antibody down to 1:740 in SEPT 2024. Thank you sir.
How to Order Your Own Spike Antibody Test
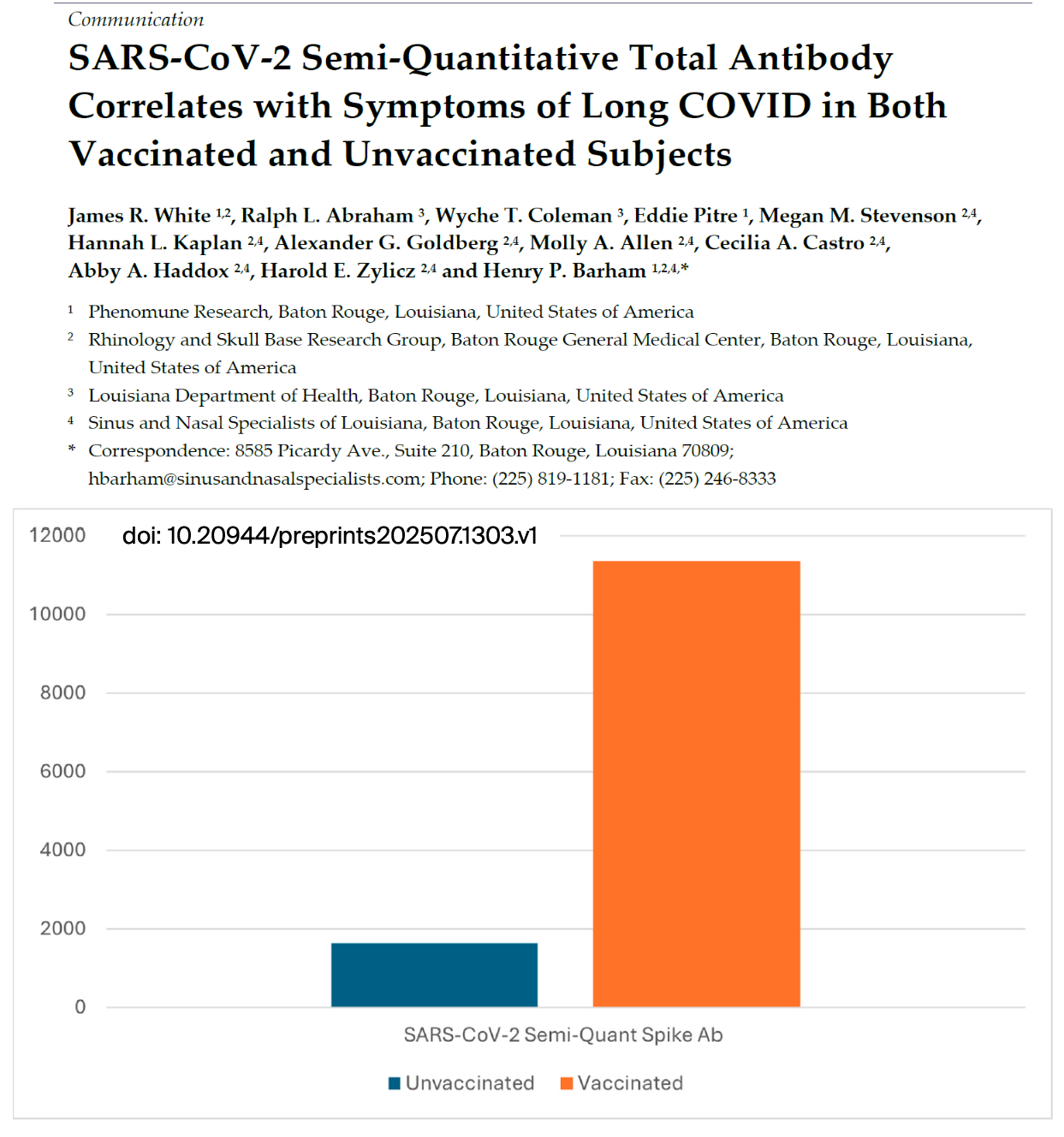
Here is a quick guide of interpretation of your results:
- <1000 U/ml very low level past exposure, negligible risks
- 1000-5000 U/ml symptoms or problem could be related to Spike protein
- >5000 U/ml Spike protein likely circulating in your bloodstream
- 10,000-25,000 U/ml very high risk for cardiac damage, blood clots, neurologic problems, autoimmunity, and potentially cancer
You can also order a Spike antibody (Covid-19 antibody) test from healthlabs.com to assess your risk and establish a baseline before and after starting any anti-spike protein protocol.
Spike Antibodies Correlate with Symptoms of Long COVID in Both Vaccinated and Unvaccinated Subjects
Wrapping Up
While it is definitely smart to be curious about spike proteins, there’s more to staying healthy. Remember, looking after your overall health is key. Eating well, staying active, and keeping stress low are big parts of this. Even though testing for spike proteins seems important, the science is still emerging. Rest assured, we will do our best to keep you updated as our understanding evolves.Sources and References:
- https://covid19criticalcare.com/can-you-test-for-spike-protein-in-the-body/
- https://www.thefocalpoints.com/p/importance-of-knowing-anti-spike
Editor's Note:
Though there are many spike protein detox treatment protocols out there, we consider and recommend the I-Recover protocol as one of the best.
Given the lack of clinical trials of long-haul COVID-19 syndrome, these recommendations are based on the abnormal changes within the body associated with the COVID-19 disease and post viral illnesses along with the collective experience of FLCCC members.









.png)

Comments
Post a Comment