Long COVID Treatment: What You Need to Know (2022)
With 200-plus symptoms linked to long COVID, treatment starts by pinpointing specific medical conditions and referring patients to the right clinicians. These might be lung specialists, heart specialists or brain rehabilitation experts.
For people with long COVID, recovery can feel like one step forward and two steps back. It’s frustrating when typical job functions or previously easy exercise – like a short walk around the block – wipe you out and you can’t get out of bed for the next two days. Long-COVID treatment protocols address that excessive fatigue.
Long COVID Symptoms
Post-COVID syndrome can encompass multiple organ systems and a wide range of symptoms including:
- Fatigue.
- Post-exertional malaise.
- Brain fog.
- Memory issues.
- Headache.
- Sleep problems.
- Shortness of breath.
- Muscle aches and joint pain.
- Speech/language issues.
- Heart palpitations.
- Tachycardia (rapid heartbeat).
- Dizziness and balance problems.
- Diarrhea and other gastrointestinal symptoms.
- Joint pain.
- Chest tightness or pain.
Wide-Ranging Long-COVID Effects
Dr. Monica Verduzco-Gutierrez is a physiatrist, professor and chair of the department of rehabilitation medicine at the Long School of Medicine at the University of Texas Health at San Antonio. She developed the Post-COVID Recovery Clinic at the UT Health Science Center at San Antonio.
“Probably one of the bigger motivators was seeing some of the disproportionate effects that COVID was having on certain populations, including those from marginalized groups and minority groups,” Verduzco-Gutierrez says. Creating the post-COVID program was important to serve the entire community.
Some patients have had severe COVID-19 disease courses that required hospitalization, Verduzco-Gutierrez says. Others might be referred to the clinic by their primary care physicians, or they refer themselves. “Some of them hear about it from social media contacts and are just trying to get as much help as they can,” she says.
Fatigue is among the most common complaints of COVID long-haulers. “Definitely, we hear a lot about fatigue,” Verduzco-Gutierrez says. “And it’s just debilitating, overwhelming fatigue. Very otherwise fit, healthy people try to go for a day at work – and they are in bed by 5:30 and can barely get up the next day.”
An international review published in August 2021 identified 203 long-COVID symptoms in 10 of the body’s organ systems. Researchers analyzed survey responses from nearly 4,000 participants and after six months, the top three symptoms were fatigue, post-exertional malaise and cognitive dysfunction. However, symptoms can occur across the board in various combinations.
“Some people feel short of breath just trying to walk around,” she says. “People are getting palpitations that are abnormal. Their blood pressure may be too high or too low. They have symptoms like numbness or tingling.” Hair loss and skin changes are also among myriad possible symptoms.
Post-COVID Screening
Dr. Robert Kotloff is a professor of medicine at the Perelman School of Medicine at the University of Pennsylvania and director of Penn Medicine’s Harron Lung Center in Philadelphia. He works with patients at the post-COVID respiratory clinic, one of the hospital’s specialty post-COVID clinics.
At Penn, patients are initially seen at the comprehensive recovery clinic run by the physical medicine and rehabilitation team. They undergo thorough screening to determine whether they’re suffering from post-COVID syndrome.
Team members “do a comprehensive assessment from head to toe, meaning symptoms of various organ systems,” Kotloff explains. “And they screen and decide if the patients then need to be sent to more specialized clinics. For instance, patients who have respiratory symptoms or respiratory issues will be sent to my clinic.”
In other cases, screening may reveal signs of heart problems like myocarditis – inflammation of the heart muscle usually caused by a viral illness. Tests such as EKGs and cardiac ECHOs are used to rule out cardiac complications of COVID-19. Depending on the results, patients may be referred to the post-COVID cardiac program.
Long COVID Treatment
Treatment for long COVID depends on individual symptoms. For the most common problems linked to long COVID, treatment and rehabilitation include the following:
- Cognition and speech-related issues. Cognitive speech therapy can help patients improve memory and attention, planning and organization, problem-solving, language and naming skills.
- Shortness of breath. Breathing exercises and respiratory therapy can gradually improve patients' lung function.
- Fatigue. Rehab with physical therapists includes encouraging patients to pace themselves, prioritize their activities and discover exercise types and duration they can endure without excessive fatigue.
- Abnormal heart rate changes. Postural orthostatic tachycardia syndrome can occur with long COVID. In POTS, people (usually women) experience a too-high increase in heart rate when they move from a lying to a standing position. As with similar conditions involving the autonomic nervous system, exercising gently, starting from a lying-down position, is important for patients who experience palpitations or rapid heartbeats.
Cognitive and Speech-Related Issues
Brain fog might be a too-mild misnomer for the significant cognitive effects that COVID long-haulers can experience, Verduzco-Gutierrez says. "They’re having really big issues with concentration and memory, trying to find words, trying to do things they did before,” she says, similar to other patients she’s seen with brain injuries.
Treatment for brain-related symptoms can be challenging. “You use some neurocognitive rehabilitation techniques,” Verduzco-Gutierrez says. “You have to try to reverse what can be reversed. You have to try to decrease inflammation that a patient may have. You have to make sure that you rule out something (else) that could be going on with the brain. You have to make sure you treat any other symptoms – like if they have headache or poor sleep – anything that could also be contributing.”
Speech can be impacted. “Some patients may be having a hard time saying what they want to say, getting the words out that they want to get out and remembering really simple words that they should already know,” Verduzco-Gutierrez says.
To guide treatment, she says, “patients (may be) referred for neuropsychological examination so that they can get really in-depth testing to see: Is it processing speed? Is it words? Is it attention? Is it executive function? And then we may send them to a neurocognitive rehabilitation program to work on those issues.”
Some patients benefit from participating in research trials on post-COVID syndrome to find out exactly what’s going on, she says.
Patients might need evaluation and treatment for new medical conditions – like diabetes or lupus – that may be caused or worsened by COVID-19. “It accelerates anything,” Verduzco-Gutierrez says. “So, if you maybe have a predisposition to high blood pressure or a predisposition to diabetes, then this may be something that really causes you to become diabetic,” or be diagnosed with hypertension.
Long-COVID Shortness of Breath
At the specialty respiratory clinic, “basically, I’m seeing two types of patients,” Kotloff says. “I’m seeing patients who were quite ill with COVID pneumonia, most of them typically hospitalized, who were then successfully discharged and who have a protracted recovery, during which the lungs have to heal from pneumonia.”
Post-COVID patients are different. “Curiously, many of these individuals have had only mild infection,” Kotloff says. “The overwhelming majority have not required hospitalization – and yet they’re plagued with lingering symptoms for many weeks to months after their acute infection.”
For “typical” COVID-19 patients who were hospitalized with severe respiratory illness, “we can point to an abnormal chest X-ray or an abnormal CT scan,” Kotloff says. “When we check their lung function studies, at least early on, they tend to be abnormal. Their oxygen levels tend to be abnormal. So, we have objective evidence to point to as to why it’s taking time for them to heal and why they’re having their symptoms.”
By contrast, shortness of breath is why most patients with post-COVID syndrome are initially referred to the respiratory clinic. “The long COVID patients, at least those who never had pneumonia, are more of a mystery because all of their traditional studies looking for respiratory causes of shortness of breath end up being normal,” Kotloff says.
Even so, almost all these long COVID patients describe the same type of shortness of breath. “Most of the post-COVID patients I’ve spoken to have either a combination of exertional and resting shortness of breath, or some of them even have exclusively resting shortness of breath.”
Instead of the usual feeling of needing to catch your breath after a run, Kotloff says, “for the post-COVID patients it’s more an uncomfortable awareness of breathing, or some will describe it as the inability to take a deep and satisfying breath.”
When treating patients recovering from pneumonia, Kotloff says, “a lot of this is what I call ‘tincture of time’ and incremental exercise to get them back on their feet.” Most will eventually recover with minimal to no effect on lung function, he says, and oftentimes they’ll benefit from enrolling in a pulmonary rehabilitation program.
Treatment for long COVID patients with shortness of breath is more complicated, he says. “It’s a bit more frustrating because what we’d like to tell them is, ‘Go out and try to exercise. Reintroduce a routine. Take a short walk and gradually increase the duration of that walk.’” However, post-exertional malaise – in which people feel fatigue markedly out of proportion to an activity – is a problem for many long COVID patients. “These patients will attempt exercise or attempt an active day and then will be totally wiped out for the next two.”
Treating Fatigue
Long COVID symptoms are often more multiplicative than additive, says Dr. Becky Lansky, a physiatrist and part of the COVID-19 recovery program at Emerson Hospital in Concord, Massachusetts. When patients complain of symptoms like brain fog or decreased concentration, she says, fatigue ties in as a major symptom.
“When you’re tired, you are more irritable,” Lansky explains. “That irritability, along with the difficulty concentrating, makes your memory worse – it sort of makes everything worse. So, many things can affect cognition.”
Determining a patient’s fatigue level helps clinicians prescribe appropriate exercise. “I believe that exercise is medicine, so everybody gets an exercise routine,” Lansky says. “But it’s very different for somebody who has difficulty walking to the bathroom as opposed to somebody who is able to walk a half-mile.”
First, it’s important to make sure that underlying physical problems aren’t contributing to excessive fatigue. “There are people who have inflammation of the heart that’s (causing) the fatigue,” Lansky says. “There are people who have decreased respiratory expansion and difficulty breathing, so there are breathing protocols to work with. There are people who have malabsorption syndrome because their gut microbiome is off, so therefore they need iron or B12.”
For other people, long COVID symptoms may be set off by pushing their bodies too hard. A graduated exercise program can meet patients where they are in terms of fatigue and other symptoms, Lansky says.
Dysautonomia
A condition called dysautonomia, a problem with the body’s control of involuntary actions, is a common long COVID symptom. “The autonomic system of the body is not working appropriately,” Lansky explains. “Which means sometimes the heart beats too quickly and sometimes the heart doesn’t beat fast enough. If that’s the case, you have to start all exercises lying down, because you don’t want to stress the heart too much.”
Working with physical and occupational therapists can help you safely resume exercise and work activities to the degree that you can tolerate.
Lifestyle Management and Long COVID
Many everyday tasks pose a challenge for long COVID sufferers. Post-COVID rehabilitation includes:
- Work limitations. Taking frequent breaks throughout the day and working with occupational therapists may make job responsibilities more manageable for some long COVID patients.
- Exercise and activities. Building stamina takes time when getting back to activity.
Managing Long COVID and Work
Work activity – even concentrating on a computer screen – can become a lot harder with long COVID. It goes beyond normal tiredness that anybody may experience after sitting at the computer for six hours or more a day, Lansky says.
With deconditioning due to being sick for a few weeks, combined with various long-COVID effects, “you fatigue significantly faster,” Lansky says. “So breaks are a critical part of recovery.”
Long-COVID treatment includes helping long haulers learn how to prioritize their health as they work. “You set your alarm and say: OK, I’m going to read emails for an hour, and then I’m going to lie down,” she says. “Then I’m going to check in with all my symptoms and see where I’m at, rest and recover and then I can go back and do some more.”
Post-COVID Exercise and Activities
Your return to physical activity should take each body system into account including the heart, lungs, blood-clotting, gastrointestinal and musculoskeletal systems. Rehabilitation experts are sharing emerging best practices for resuming activity after COVID, including for people with long COVID:
- Have a comprehensive medical evaluation.
- Avoid being entirely sedentary or immobile, which can affect circulation and muscle health.
- Return gradually to activity in a slow, stepwise manner.
- Talk to your health care provider about any symptoms that occur with exertion.
- Pace yourself and dial down physical or work activities that cause excessive fatigue.
- Break daily activities up into smaller tasks throughout the day, as tolerated.
- Practice deep breathing to help restore lung function compromised by COVID-19.
- Incorporate breaks into daily work routines.
The American Academy of Pediatrics provides guidelines for children and adolescents with COVID-19 returning to sports and physical activity.
Seeking Treatment for Long COVID
Just how long does long-COVID last? Patients who experience long COVID may have symptoms for a year or more after their initial COVID-19 infection, according to a study of 156 participants, published in the January 2022 issue of the American Journal of Physical and Rehabilitation Medicine. These persistent symptoms can significantly affect patients’ cognition, their ability to work or participate in physical activity, their interactions with others and their overall quality of life. Nearly half of the study participants who had worked full-time before COVID-19 no longer did.
If you previously had even a mild COVID-19 infection but still don’t feel well, it’s better to address it early, Verduzco-Gutierrez emphasizes.
Most states have at least one post-COVID care clinic, often located at large teaching hospitals. You can find clinics nearest you through an online directory provided by Survivor Corps, an organization that helps people with long COVID.
Additional Long COVID Treatment Strategies
- The FLCCC treatment protocol — The Frontline COVID-19 Critical Care Alliance (FLCCC) has developed protocols both for those struggling with long COVID and those injured by the COVID jabs. You can download both from covid19criticalcare.com.
- Time-restricted eating (TRE) can help eliminate the toxic proteins by stimulating autophagy, and nattokinase, a form of fermented soy, is helpful for reducing blood clots, Several additional detox remedies can be found in “World Council for Health Reveals Spike Protein Detox.”
- Dr. Peter McCullough reports having had some success treating neurological symptoms with fluvoxamine, an SSRI antidepressant, and a March 2022 review paper24 suggests combating the neurotoxic effects of the spike protein using the flavonoids luteolin and quercetin.
- An international collaboration involving researchers in Israel and the U.S. has also developed what they claim is a “breakthrough” proprietary nutritional formula for long COVID called “Restore”. Study results suggest each of the reported symptoms were alleviated in 72% to 84% of study participants after four weeks of standalone use. The supplement contains nutrients and plant bio-extracts for critical immune restoration after surviving a viral infection, with ingredients including zinc, vitamin D, quercetin, bromelain, St. John’s wort, Indian frankincense and beta caryophyllene, a cannabinoid CB2 agonist.
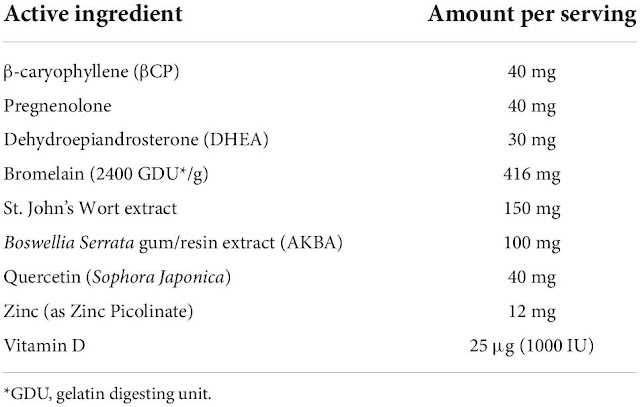 |
| Restore from NViroMune: Amount of each compound included in the nutraceutical formulation per serving. The participants were required to take one serving twice a day with food. |
Republished and updated from:
https://health.usnews.com/conditions/coronavirus-and-your-health/articles/long-covid-treatments







.png)

Comments
Post a Comment