Omicron subvariant XBB.1.5 prevalence jumps to 74% in US: Symptoms and Treatment
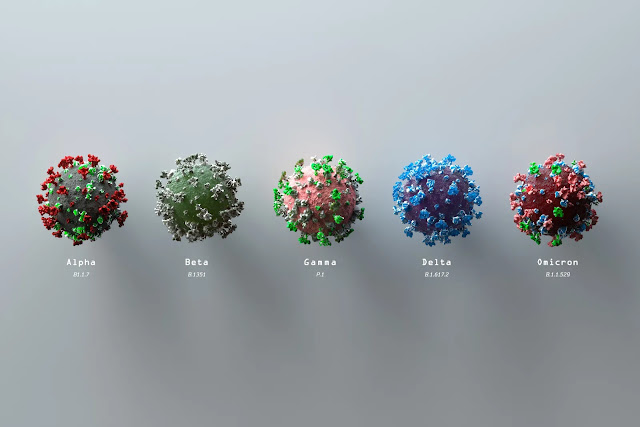
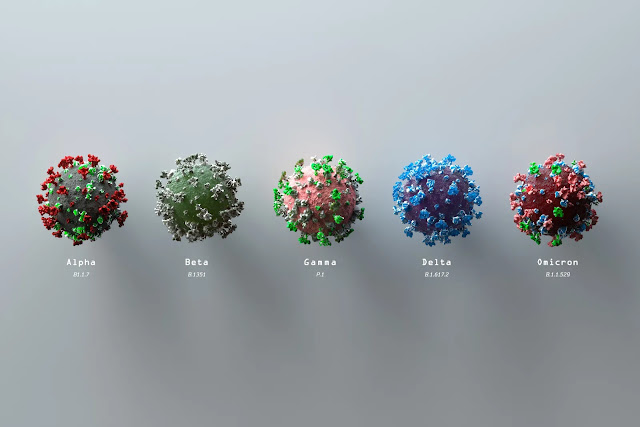
XBB.1.5 omicron subvariant has overtaken BQ.1.1 and BQ.1 as the prevailing version of the coronavirus in the United States.
XBB.1.5, now accounts for 74.7% of confirmed COVID-19 cases in the United States, according to the most recent estimates from the U.S. Centers for Disease Control and Prevention (week ending Feb 11, 2023).
The new variant, XBB.1.5, was dubbed the "Kraken," which is a moniker referring to a legendary sea beast that could not be defeated. As reported by NBC Chicago:
"A highly contagious 'recombinant' variant composed of two different BA.2 strains, the 'kraken' variant has quickly become the dominant form of COVID in the U.S. and is continuing to spread nationwide. Also known as XBB.1.5, the variant quickly rose to prominence as experts say it is more contagious than many of its predecessors.
'It went from 4% of sequences to 40% in just a few weeks,' Dr. Ashish Jha, White House COVID czar, tweeted last week. 'That's a stunning increase.' Jha said the variant is likely more immune evasive, even 'more than other omicron variants.'"
"Arwady noted symptoms haven't changed with the new variant, though she noted that symptoms similar to the flu are less common … 'COVID is showing up very much like it already has. I think, if anything, we are seeing it a little bit less likely to have the more severe symptoms,' Arwady said.
'Definitely people get the severe symptoms still … But more often now we are seeing people … just have cold-like symptoms, less likely to have those flu-like, really feeling very sick, the high fevers.'"
This is entirely logical, as XBB.1.5 is a recombination of two Omicron strains, and as Dr. Dennis Cunningham, medical director of infection control and prevention at Henry Ford Health in Detroit told NBC Chicago:
"The omicron symptoms have been pretty consistent. There's less incidence of people losing their sense of taste and smell. In a lot of ways, it's a bad cold, a lot of respiratory symptoms, stuffy nose, coughing, body aches and fatigue … I haven't seen anything suggesting that this new subvariant [XBB.1.5] is clearly making people sicker."

But why the "kraken" variant? Dr. Ryan Gregory, a biology professor at the University of Guelph in Ontario, Canada, said the nickname was simply "intended to help people keep track of who's who in the ever-growing variant soup."
In a tweet, Gregory stressed the nickname was "informal." Previous variants have also been given nicknames like the "nightmare" or "scrabble" variants.
It evolved from the XBB family of variants, which started driving outbreaks during the fall in Singapore and other parts of Asia, Dr. Andy Pekosz, a virologist at Johns Hopkins University.
"The XBB.1.5 appears to have first been detected sometime in November, although that’s still a little bit hazy as people are sequencing more viruses," Pekosz explains.
"It really started to come into play in December 2022 in terms of having this exponential growth of cases here in the U.S.," says Pekosz, adding that holiday travel and gatherings are likely contributing to the surge in cases.
While there is still a lot we don't know about XBB.1.5, the data available so far suggest that XBB.1.5 is more transmissible or infectious than other omicron variants, says Al-Aly.
In a WHO press conference on Jan. 4, the WHO technical lead on COVID-19, Dr. Maria Van Kerkhove, called XBB.1.5 "the most transmissible subvariant that has been detected yet." Kerkhove added that XBB.1.5 has "rapidly replaced other circulating variants" in the Northeastern U.S. and WHO expects "further waves of infection around the world."
"XBB.1.5 became dominant so quickly based on its ability to escape from existing immunity and its enhanced ability to bind to host cells and infect them," Akiko Iwasaki, Ph.D., director of the Center for Infection & Immunity at the Yale School of Medicine.
The XBB family of variants have a lot of mutations, says Pekosz, but XBB.1.5 picked up an extra mutation that allows the virus to adhere better to cells in the respiratory tract and replicate easily.
Regarding the existing immunity aspect, the body produces antibodies that detect and fight off the virus, per the CDC, which protect you from getting sick in the future. "In people who have been vaccinated or boosted, or previously infected with SARS-CoV-2, we operate under the assumption that they may carry some immunity," Al-Aly explains.
However, XBB.1.5 is better at dodging these antibodies, which is not new with the XBB family. "XBB.1.5 appears to be just as immune evasive as the XBB and XBB.1, which are more evasive of antibodies ... than other omicron subvariants," says Iwasaki.
"The omicron symptoms have been pretty consistent. There's less incidence of people losing their sense of taste and smell. In a lot of ways, it's a bad cold, a lot of respiratory symptoms, stuffy nose, coughing, body aches and fatigue … I haven't seen anything suggesting that this new subvariant [XBB.1.5] is clearly making people sicker."

But why the "kraken" variant? Dr. Ryan Gregory, a biology professor at the University of Guelph in Ontario, Canada, said the nickname was simply "intended to help people keep track of who's who in the ever-growing variant soup."
In a tweet, Gregory stressed the nickname was "informal." Previous variants have also been given nicknames like the "nightmare" or "scrabble" variants.
What is XBB.1.5 variant?
Omicron XBB.1.5 is a recombinant (or a hybrid) of two omicron sublineages that descended from another omicron subvariant called BA.2, according to experts at the World Health Organization. It has been detected in 29 countries so far.It evolved from the XBB family of variants, which started driving outbreaks during the fall in Singapore and other parts of Asia, Dr. Andy Pekosz, a virologist at Johns Hopkins University.
"The XBB.1.5 appears to have first been detected sometime in November, although that’s still a little bit hazy as people are sequencing more viruses," Pekosz explains.
"It really started to come into play in December 2022 in terms of having this exponential growth of cases here in the U.S.," says Pekosz, adding that holiday travel and gatherings are likely contributing to the surge in cases.
While there is still a lot we don't know about XBB.1.5, the data available so far suggest that XBB.1.5 is more transmissible or infectious than other omicron variants, says Al-Aly.
In a WHO press conference on Jan. 4, the WHO technical lead on COVID-19, Dr. Maria Van Kerkhove, called XBB.1.5 "the most transmissible subvariant that has been detected yet." Kerkhove added that XBB.1.5 has "rapidly replaced other circulating variants" in the Northeastern U.S. and WHO expects "further waves of infection around the world."
How did XBB.1.5 become dominant so quickly?
The XBB family of variants have a lot of mutations, says Pekosz, but XBB.1.5 picked up an extra mutation that allows the virus to adhere better to cells in the respiratory tract and replicate easily.
Regarding the existing immunity aspect, the body produces antibodies that detect and fight off the virus, per the CDC, which protect you from getting sick in the future. "In people who have been vaccinated or boosted, or previously infected with SARS-CoV-2, we operate under the assumption that they may carry some immunity," Al-Aly explains.
However, XBB.1.5 is better at dodging these antibodies, which is not new with the XBB family. "XBB.1.5 appears to be just as immune evasive as the XBB and XBB.1, which are more evasive of antibodies ... than other omicron subvariants," says Iwasaki.
Are the symptoms of XBB.1.5 more severe?
“So far, the symptoms are very similar to other variants, (and) increases in hospitalizations seem to be focused on the elderly, who have always been more susceptible to severe COVID," says Pekosz.XBB, is a hybrid between two descendants of the BA.2 version of Omicron (WHO). A World Health Organisation press release on XBB states: “While further studies are needed, the current data do not suggest there are substantial differences in disease severity for XBB infections. There is, however, early evidence pointing at a higher reinfection risk, as compared to other circulating Omicron sublineages.”
Some of the most common COVID-19 symptoms at this stage in the pandemic, include:
"Even if it's less severe, if it's more transmissible, (then) it affects a whole lot of people — that could still fill up hospitals and also potentially increase the rates of death," says Al-Aly. This is especially true for high-risk or immunocompromised groups, the experts note.
XBB.1.5's mutations do not seem to affect the part of the virus that is targeted by the COVID-19 antiviral treatment Paxlovid. "There is no reason for us to believe that it won't respond to existing antivirals," Dr. Ziyad Al-Aly, a clinical epidemiologist at Washington University in St. Louis, tells TODAY.com.
That said, we do not know exactly how XBB.1.5 will compare to other omicron subvariants with respect to symptoms and severity yet, says Iwasaki. As with any new variant, we will learn more about XBB.1.5 as more data becomes available.
“The more (the coronavirus) circulates, the more opportunities it will have to change,” Van Kerkhove pointed out at the WHO press conference.
"It is distinct enough from some of the earlier omicron variants, like BA.1 and BA.5, for example, that you could theoretically get reinfected with this XBB.1.5 even if you had an earlier omicron infection," says Pekosz.
"Also over time your immune response gets reduced, and that makes it even more likely that you'll get infected," says Pekosz. So even if you had a decent immune response to omicron, by two or three months later, it will decrease and it'll be easier XBB.1.5 to be able to infect you, Pekosz adds.
Al-Aly calls the immune-evasive feature "alarming" because it may increase the risk of reinfection, which experts agree people should try to avoid.
“Repeated infections with SARS-CoV-2 appear to increase the risk for long COVID,” says Iwasaki, citing a study in Nature Medicine.
"It might evade vaccine-induced immunity, but that doesn't mean that vaccines will all of a sudden stop protecting you. ... It just means the effectiveness is diminished," says Al-Aly, adding that being vaccinated and boosted is still absolutely safer than being unvaccinated.
"You would want to have a vaccine that’s specifically tailored to XBB.1.5, but we don’t have that (yet) — the only thing that we have right now is the bivalent booster," says Al-Aly. So it's still a good idea to be up to date on your vaccinations and boosters if you're not already.
In the meantime, you can also protect yourself and others from COVID-19 by practicing everyday precautions, like wearing a mask, avoiding crowded indoor spaces and staying home when sick, Al-Aly says.
"I think (XBB.1.5) is a reminder that this virus is going to continue to be with us, and that we're going to have to double our efforts to use the tools that we have to limit the impact of infection," says Pekosz.
It is important to consult with a healthcare provider and start treatment as soon as you experience symptoms of COVID-19. Delaying treatment may increase your risk of experiencing severe symptoms. In addition to seeking medical treatment, it is important to follow guidelines from the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), and local authorities, such as wearing a mask, practicing social distancing, getting vaccinated, and avoiding crowds. Implementing multiple prevention strategies can help protect against COVID-19 and minimize your risk.
Some of the most common COVID-19 symptoms at this stage in the pandemic, include:
- Sore throat
- Fever or chills
- Runny nose
- Blocked nose
- Sneezing
- Cough without phlegm (a dry cough)
- Headache
- Cough with phlegm (a wet cough)
- Hoarse voice
- Muscle aches and pain
- Altered sense of smell
- Itchy throat
"Even if it's less severe, if it's more transmissible, (then) it affects a whole lot of people — that could still fill up hospitals and also potentially increase the rates of death," says Al-Aly. This is especially true for high-risk or immunocompromised groups, the experts note.
XBB.1.5's mutations do not seem to affect the part of the virus that is targeted by the COVID-19 antiviral treatment Paxlovid. "There is no reason for us to believe that it won't respond to existing antivirals," Dr. Ziyad Al-Aly, a clinical epidemiologist at Washington University in St. Louis, tells TODAY.com.
That said, we do not know exactly how XBB.1.5 will compare to other omicron subvariants with respect to symptoms and severity yet, says Iwasaki. As with any new variant, we will learn more about XBB.1.5 as more data becomes available.
“The more (the coronavirus) circulates, the more opportunities it will have to change,” Van Kerkhove pointed out at the WHO press conference.
Can you get XBB.1.5 after having another omicron variant?
Yes, and one can't necessarily assume that prior infection — even in the last several months — will protect you, the experts note."It is distinct enough from some of the earlier omicron variants, like BA.1 and BA.5, for example, that you could theoretically get reinfected with this XBB.1.5 even if you had an earlier omicron infection," says Pekosz.
"Also over time your immune response gets reduced, and that makes it even more likely that you'll get infected," says Pekosz. So even if you had a decent immune response to omicron, by two or three months later, it will decrease and it'll be easier XBB.1.5 to be able to infect you, Pekosz adds.
Al-Aly calls the immune-evasive feature "alarming" because it may increase the risk of reinfection, which experts agree people should try to avoid.
“Repeated infections with SARS-CoV-2 appear to increase the risk for long COVID,” says Iwasaki, citing a study in Nature Medicine.
Can I get XBB.1.5 if I'm vaccinated and boosted?
It's possible to get XBB.1.5 even if you're vaccinated and boosted, says Al-Aly. However, the current COVID-19 vaccine and the bivalent booster (which targets BA.4 and BA.5) still provide protection against omicron variants and severe disease, the experts note."It might evade vaccine-induced immunity, but that doesn't mean that vaccines will all of a sudden stop protecting you. ... It just means the effectiveness is diminished," says Al-Aly, adding that being vaccinated and boosted is still absolutely safer than being unvaccinated.
"You would want to have a vaccine that’s specifically tailored to XBB.1.5, but we don’t have that (yet) — the only thing that we have right now is the bivalent booster," says Al-Aly. So it's still a good idea to be up to date on your vaccinations and boosters if you're not already.
In the meantime, you can also protect yourself and others from COVID-19 by practicing everyday precautions, like wearing a mask, avoiding crowded indoor spaces and staying home when sick, Al-Aly says.
"I think (XBB.1.5) is a reminder that this virus is going to continue to be with us, and that we're going to have to double our efforts to use the tools that we have to limit the impact of infection," says Pekosz.
Take a Test
How well do our tests work on XBB.1.5? All the evidence says that they should work just fine, according to Dr. Ashish Jha, the White House COVID-19 response coordinator, in a Jan. 4, 2023 Twitter thread.Every U.S. household is eligible to order 4 free at-home COVID-19 tests. (covidtest.gov)
Between 48 and 72 hours after potential COVID exposure or at the first sign of any symptoms, people should take either a rapid antigen or PCR test. “There should be a very low threshold for testing yourself to see whether you have COVID or whether you have something else,” says Amesh Adalja, a senior scholar at the Johns Hopkins Center for Health Security. COVID can look very like a cold, influenza or allergies, but the treatments for each are different.
PCR tests are more sensitive but harder to get, and taking a rapid antigen test at home usually suffices, the experts say. If the first test is negative, people should wait two days (behaving cautiously in the meantime) and take another one. If it is COVID, the viral load will increase in that time. “Nothing in life is perfect, nor are the rapid antigen tests, but they’re pretty darn good at picking up contagious levels of virus,” says Lucy McBride, a practicing primary care doctor in Washington, D.C. (Lists of free test locations are available on the Test to Treat locator Web site provided by the U.S. Department of Health and Human Services.)
When people test positive, it is a good idea for them to call a primary care physician if they have one. Doctors can provide guidance on treatment and update medical histories. They will also report the result to public health authorities so that it is included in case counts. At a minimum, people should track the date that symptoms began and the date of a positive test.
PCR tests are more sensitive but harder to get, and taking a rapid antigen test at home usually suffices, the experts say. If the first test is negative, people should wait two days (behaving cautiously in the meantime) and take another one. If it is COVID, the viral load will increase in that time. “Nothing in life is perfect, nor are the rapid antigen tests, but they’re pretty darn good at picking up contagious levels of virus,” says Lucy McBride, a practicing primary care doctor in Washington, D.C. (Lists of free test locations are available on the Test to Treat locator Web site provided by the U.S. Department of Health and Human Services.)
When people test positive, it is a good idea for them to call a primary care physician if they have one. Doctors can provide guidance on treatment and update medical histories. They will also report the result to public health authorities so that it is included in case counts. At a minimum, people should track the date that symptoms began and the date of a positive test.
Over-the-Counter Help
Most people who get COVID will be just fine at home. “If you’re vaccinated and boosted and generally healthy, people do very well,” McBride says. Over-the-counter medications will not treat COVID directly but can help manage symptoms. Doctors recommend acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil or Motrin) to bring down fevers and relieve achiness. Early in the pandemic, there were reports that ibuprofen made COVID worse, but those have not been substantiated. NSAIDs are only intended to be taken for short periods, however, because they have more side effects than acetaminophen, and they are not safe for everyone. People who take other medications should consult with a doctor before taking NSAIDs. Antihistamines or cold medications such as DayQuil can be used to relieve congestion and cough.Getting enough rest is critical, as is drinking enough fluids, which prevent dehydration and reduce cough.
Having a pulse oximeter at home would also be useful to calculate the amount of oxygen in a person’s blood without having to draw a blood sample. If oxygen levels fall below 95 per cent, that would be a sign to visit the hospital.
Thermometers, tissues and hand sanitizer are other supplies often recommended to keep at home while experiencing a COVID-19 infection. Finally, it won’t hurt to take vitamin supplements as deficiencies might be associated with the severe form of COVID-19.
Using Prescription Drugs
One of the most significant recent changes in the COVID landscape is the wider availability of authorized outpatient treatments. The antiviral drug Paxlovid reduced risk of hospitalization and death by 89 percent in a clinical trial, and it is a pill, which makes it relatively easy to take. The drug cannot be taken with many common medications such as statins or blood thinners, however. Paxlovid is available by prescription or at Test to Treat sites nationwide for people who are eligible.Omicron variant XBB found to be resistant to monoclonal antibody treatments
According to the authors from a study, published in the New England Journal of Medicine (Dec 2022).:
"...These results suggest that imdevimab–casirivimab, tixagevimab–cilgavimab, sotrovimab, and bebtelovimab may not be effective against BQ.1.1 or XBB in the clinical setting...These results suggest that remdesivir, molnupiravir, and nirmatrelvir are efficacious against both BQ.1.1 and XBB in vitro..."
XBB.1.5 is slightly different from its relatives, because it not only evades protective antibodies, it also is better at binding to cells. That means healthy adults are more likely to be infected with it even after vaccination or an infection with a different variant.
But other parts of the immune system can still come to our defense, Dr. Otto Yang, an infectious disease physician and immunology researcher at David Geffen School of Medicine at the University of California, Los Angeles, told The New York Times.
Even if mutations in some parts of the virus prevent antibodies from blocking an infection, T cells should be able to recognize the main part of the virus spike protein, Dr. Yang said. And because T cells remember how to respond to the coronavirus based on what they’ve learned from previous encounters or vaccines, they can mount an attack quickly if you do become infected. “They are what prevent severe illness,” Dr. Yang said. “People who are up to date on their vaccines and who get treatment early with Paxlovid or with remdesivir are going to do fine, for the most part.” (Paxlovid is an oral antiviral medication, and remdesivir is an injectable one.)
Immune evasion and infection are a bigger concern for people who are immunocompromised or who do not mount a strong immune response to vaccines. That includes people who have had stem cell or solid organ transplants, people receiving cancer treatments, people with autoimmune diseases and people who need immunosuppressive medication for various medical conditions, said Dr. Alpana Waghmare, an infectious disease expert at Fred Hutchinson Cancer Center.
The antibody treatments that many immunocompromised people have relied on, like the preventive shot Evusheld and the intravenous Covid treatment bebtelovimab, are not effective against XBB.1.5 and other new subvariants. As a result, immunocompromised people may have more severe disease, but other antiviral treatments will most likely keep deaths from increasing in this group.
XBB.1.5 is slightly different from its relatives, because it not only evades protective antibodies, it also is better at binding to cells. That means healthy adults are more likely to be infected with it even after vaccination or an infection with a different variant.
But other parts of the immune system can still come to our defense, Dr. Otto Yang, an infectious disease physician and immunology researcher at David Geffen School of Medicine at the University of California, Los Angeles, told The New York Times.
Even if mutations in some parts of the virus prevent antibodies from blocking an infection, T cells should be able to recognize the main part of the virus spike protein, Dr. Yang said. And because T cells remember how to respond to the coronavirus based on what they’ve learned from previous encounters or vaccines, they can mount an attack quickly if you do become infected. “They are what prevent severe illness,” Dr. Yang said. “People who are up to date on their vaccines and who get treatment early with Paxlovid or with remdesivir are going to do fine, for the most part.” (Paxlovid is an oral antiviral medication, and remdesivir is an injectable one.)
Immune evasion and infection are a bigger concern for people who are immunocompromised or who do not mount a strong immune response to vaccines. That includes people who have had stem cell or solid organ transplants, people receiving cancer treatments, people with autoimmune diseases and people who need immunosuppressive medication for various medical conditions, said Dr. Alpana Waghmare, an infectious disease expert at Fred Hutchinson Cancer Center.
The antibody treatments that many immunocompromised people have relied on, like the preventive shot Evusheld and the intravenous Covid treatment bebtelovimab, are not effective against XBB.1.5 and other new subvariants. As a result, immunocompromised people may have more severe disease, but other antiviral treatments will most likely keep deaths from increasing in this group.
Other At-Home Treatments
You can find a listing of doctors who can prescribe necessary home isolation medications on Find a Provider post.
There are many COVID-19 treatment protocols out there on the internet. We have reviewed many protocols and believe the FLCCC I-CARE protocol (constantly updated) is the easiest and effective to follow.
Always consult your trusted medical professional before you take any medication or supplement.
Emergency warning signs
Individuals are reminded to seek immediate medical attention (go to a hospital’s emergency department) if they develop emergency warning signs of COVID-19 such as:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- Bluish lips or face
- New confusion or inability to arouse
- Pulse oximeter reading below 95 percent (oxygen level)
Key Takeaway
Disclaimer:
- Always see or talk to your doctor before taking any drugs, supplements and over the counter products.
Z-Stack Supplement
In an effort to make it easier for patients, Dr Zelenko has developed an oral supplement that contains all four key ingredients: vitamin C, quercetin, vitamin D3 and zinc. It’s referred to as 'Z-Stack Supplement. Z-Stack Vitamin cocktail provides key ingredients needed in order to help your body fight off this deadly invader. Studies have shown that treatment needs to be started 'early'. Don't wait until it's too late to start treatment – keep a bottle on hand for peace of mind.
Z-Stack Vitamin cocktail provides key ingredients needed in order to help your body fight off this deadly invader. Studies have shown that treatment needs to be started 'early'. Don't wait until it's too late to start treatment – keep a bottle on hand for peace of mind.
The Z-Stack Vitamins are Kosher certified, GMP certified and made in the USA.
The cost of the Z-STACK vitamin cocktail is $55 per bottle for a one month supply.
Where to buy Z-Stack: Z-stack is available on Dr Zelenko's website. Here is the link: Z Stack Supplement.
Note: To get 5% OFF, please use this coupon code: drfrancis
In an effort to make it easier for patients, Dr Zelenko has developed an oral supplement that contains all four key ingredients: vitamin C, quercetin, vitamin D3 and zinc. It’s referred to as 'Z-Stack Supplement.

Z-Stack Vitamin cocktail provides key ingredients needed in order to help your body fight off this deadly invader. Studies have shown that treatment needs to be started 'early'. Don't wait until it's too late to start treatment – keep a bottle on hand for peace of mind.
The Z-Stack Vitamins are Kosher certified, GMP certified and made in the USA.
The cost of the Z-STACK vitamin cocktail is $55 per bottle for a one month supply.
The cost of the Z-STACK vitamin cocktail is $55 per bottle for a one month supply.
Where to buy Z-Stack: Z-stack is available on Dr Zelenko's website. Here is the link: Z Stack Supplement.
Note: To get 5% OFF, please use this coupon code: drfrancis






.png)

Comments
Post a Comment