Natural Ways to Increase Autophagy and Detox Spike Proteins After COVID Infection
At least 10 to 30 percent of individuals infected by SARS-CoV-2 have experienced post-COVID syndrome (also known as long-hauler syndrome, or long COVID). In the United States, 18 to 19 percent (nearly 1 in 5) of adults who reported ever having had COVID-19 currently have symptoms of long COVID, defined as symptoms lasting three or more months that were not present prior to having COVID-19.
“Post-COVID-vaccine syndrome,” a newly coined term by Dr. Paul Marik, is defined as the temporal correlation between receiving a COVID-19 vaccine and the beginning or worsening of clinical manifestations which are sufficient to diagnose a COVID-19 vaccine-induced injury when symptoms cannot be explained by other concurrent causes.
Both types of diseases have contributed to the fact that 8 percent (nearly 1 in 13) of U.S. adults, regardless of prior COVID-19 infection, currently have post-COVID-like conditions.
As a matter of fact, there are significant overlaps between long COVID and post-vaccine syndromes. Both are systemic, chronic diseases characterized by immune dysregulation, inflammation, fatigue, and declined functions of multiple vital organs, including at least the brain, heart, lungs, and endocrine organs.
According to a systematic review published in 2022 involving 1,680,003 COVID-19-positive patients from 50 studies, among the top 18 frequent symptoms of long COVID, 50 percent of them are neuropsychiatric, including brain fog, memory problems, sleep disorder, anxiety, depression, smell or taste disorders, dizziness, and headaches.
Of all the post-marketing adverse events reported by Pfizer on its COVID vaccine, neurological disorders rank second, just behind “general disorders,” followed by musculoskeletal, gastrointestinal, and respiratory issues.
These clear similarities between long COVID and COVID vaccine-induced injuries indicate that they share common pathological features as well.
Persistent Spike Protein Causes Persistent Immune Dysregulation
The spike protein-induced dysregulated inflammatory state and subsequent multiple organ damage, or proposed “spikopathy,” is indeed one of the most fundamental injuries of both syndromes.
Researchers have proven that the spike protein decreases natural killer (NK) cells and inhibits their activity. This means that the spike protein itself is able to compromise innate antiviral immunity, exhausting NK cells’ functions.
Scientists found that the spike protein could be detected in the blood mononuclear cells of long COVID patients for up to 15 months post-infection. This is associated with abnormal types of monocytes, which were presumed to be a major source of triggering chronic inflammation.
Furthermore, the SARS-CoV-2 virus can interfere with the cellular recycling process known as autophagy.
What is autophagy? Why is it important?
Autophagy: Human Self-Renewal and Self-Cleaning Process
The process of getting rid of waste or toxins from cells is called autophagy.
The concept of autophagy was first introduced in 1974 by Belgian cytologist and biochemist Christian de Duve. He was awarded the Nobel Prize in Physiology or Medicine in the same year for his discovery of lysosomes.
Literally, autophagy means “self-eating.” It is a natural physiological mechanism wherein dysfunctional cells are broken down and their waste products are used to make healthy cells, similar to a city’s waste recycling process.
During the process of autophagy, an autophagosome is first produced in the cell and then acts as a “garbage bag,” enveloping the various waste products in the cell. The “garbage bag” will fuse with a lysosome (which contains loads of enzymes to break down the garbage) to form a “garbage processing station” called an autolysosome, which will then break down and recycle the waste materials.
Once autophagy is initiated, cytoplasmic elements, or the “cargo” that is to be recycled, are engulfed into double-membrane vesicles, termed autophagosomes, which fuse with lysosomes to form autolysosomes, where the cargo is then degraded.
Autophagy is an important physiological mechanism that not only removes harmful components from cells in a timely manner but also transforms useless proteins into recyclable amino acids.
This brings a variety of benefits to the body, including anti-aging benefits, reduced inflammatory status, boosted immunity, and reduced cancer risk.
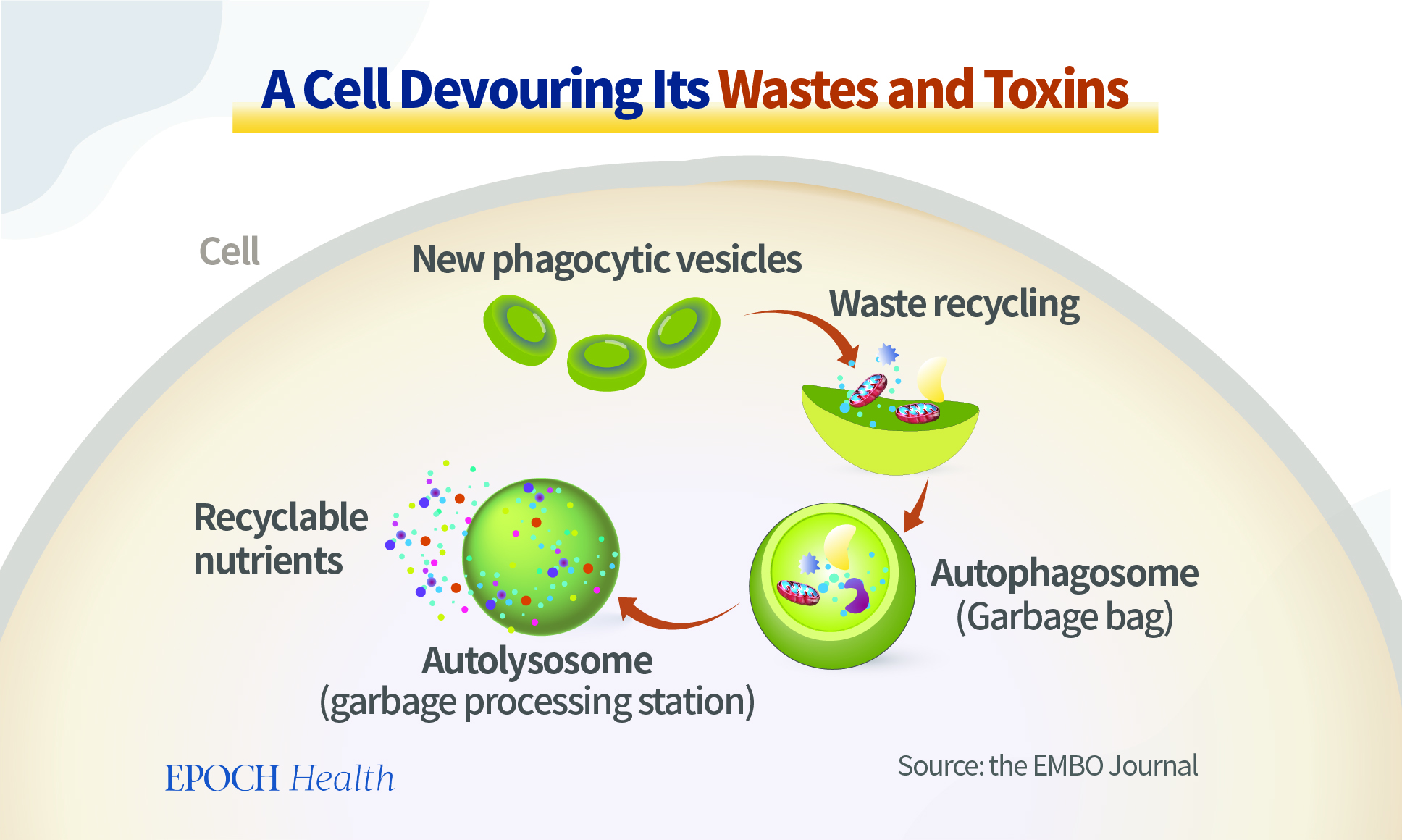 |
| Figure 1 Analog of Autophagy-Waste Recycling System |
How does SARS-CoV-2 impair autophagy?
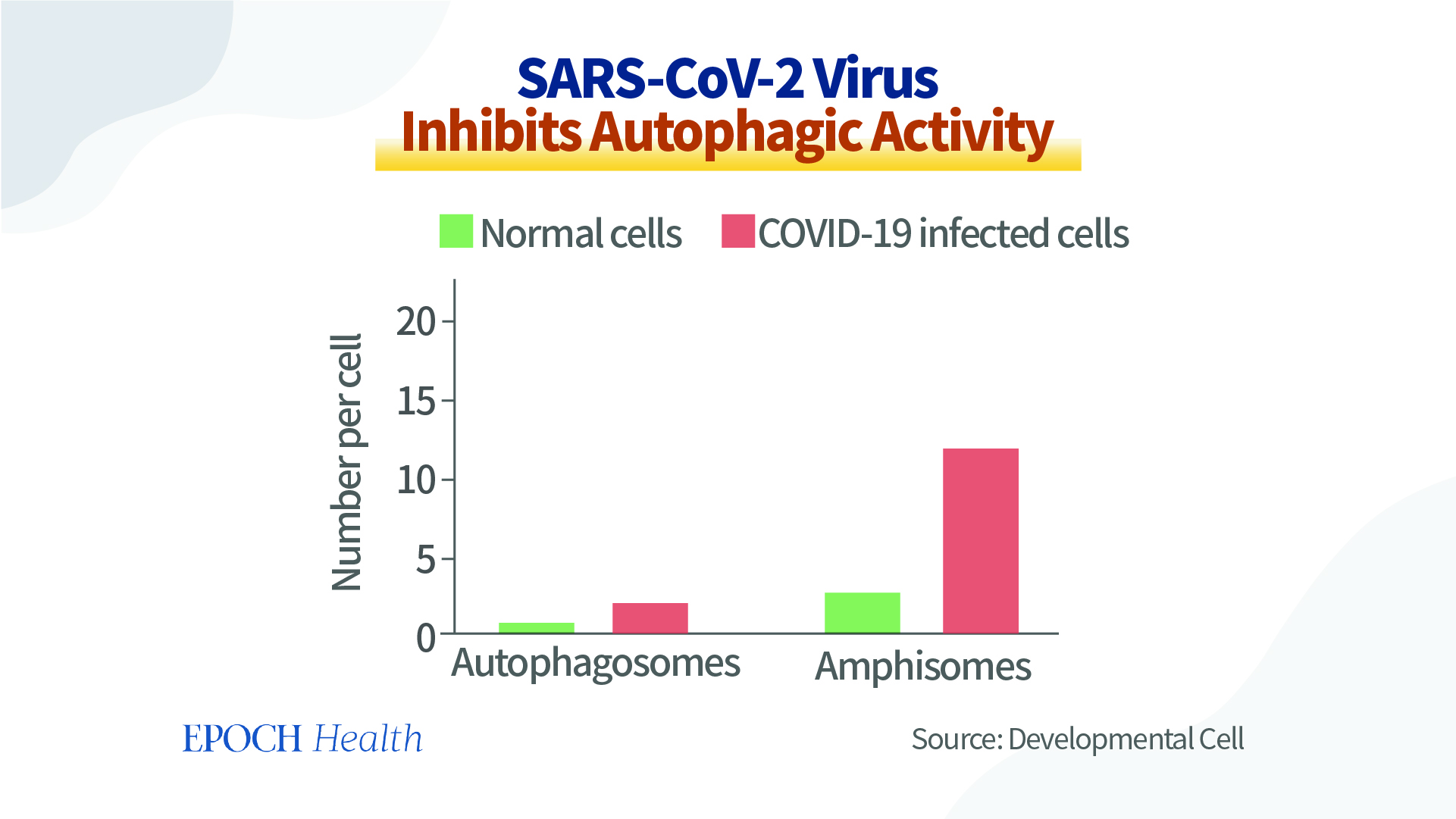 |
| Figure 2 SARS-CoV-2 Inhibits Autophagy. (Source: https://www.cell.com/developmental-cell/fulltext/S1534-5807(20)31016-9) |
A component of the SARS-CoV-2 virus (ORF3a) inhibits the cells’ waste-recycling process. The virus also impairs autophagy by reducing glycolysis and protein translation by limiting the activation of AMP-protein activating kinase (AMPK) and mammalian target of rapamycin complex 1 (mTORC1).
In cells infected with the SARS-CoV-2 virus, the formation of autolysosomes (“garbage processing stations”) has been substantially blocked, resulting in many more “garbage bags” of cellular waste accumulating inside the cells, while at the same time reducing the cells’ processing ability, preventing the timely recycling of waste and harmful substances in the cells. This further worsens the persistence of spike proteins in our bodies and cells.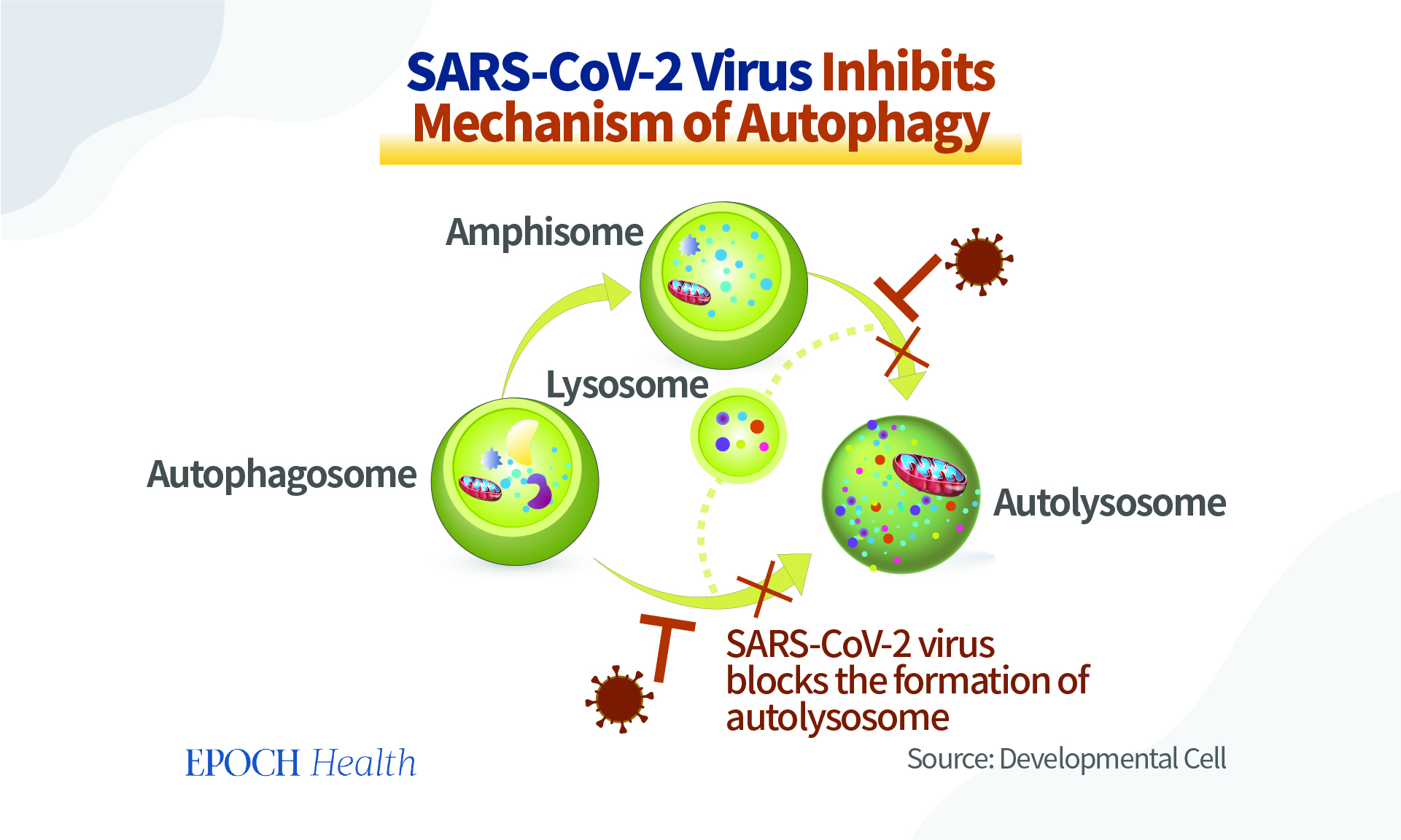 |
| Figure 3 SARS-CoV-2 Inhibits Autophagy-Cell Waste Recycling Process. (Source: https://www.cell.com/developmental-cell/fulltext/S1534-5807(20)31016-9) |
With the majority of the world’s population having been vaccinated due to policies that were put in place, it is estimated that most patients with long COVID are likely also vaccinated. This could make the symptoms of long COVID patients more complicated.
Healthy Lifestyles Boost Autophagy
As the majority of the disorders are directly or indirectly caused by the spike protein of the virus, one of the most important treatment strategies is to help eliminate the spike protein from our cells.
The most powerful way to boost our autophagy process resides with our lifestyles. For example, how much and how often do we eat? Do we go to sleep on time and get quality sleep? Do we go outside regularly to enjoy the sun? All these correlate to the level of autophagy inside our bodies.
Intermittent Fasting
Food has been considered a means of providing nutrients to people. Most people consume three meals a day, but perhaps few have the thought that three meals per day may not be necessary.
In fact, we can live even healthier if we eat a little less. Why?
After meals, our gut absorbs glucose, amino acids, and fatty acids to be used as the main sources of energy and nutrients by our cells.
During fasting, the reduced amount of glucose and amino acids downregulate a molecular pathway (called mTOR) and subsequently up-regulates autophagy.Short-term fasting leads to a dramatic upregulation in autophagy. The increased neuronal autophagy is revealed by changes in autophagosome abundance, and by diminished neuronal mTOR activity in vivo.
Mechanistically speaking, stimulating the clearance of damaged cells (autophagy), damaged mitochondria (mitophagy), and misfolded and foreign proteins has a profound effect on promoting immune system homeostasis, improving mitochondrial health, and boosting neuroregeneration.
Preclinical studies have shown robust evidence that intermittent fasting has broad-spectrum benefits for many health conditions, such as obesity, diabetes mellitus, cardiovascular disease, cancers, and neurologic disorders.
Clinical trials of intermittent fasting have shown improved verbal memory, working memory, and cognitive function. This is mainly contributed by the enhanced autophagy processes that help neuronal cells clear their waste more efficiently.
Fasting also triggers the breakdown of triglycerides, resulting in increased levels of free fatty acids (FFA), which subsequently generate more ATP as well as more proteins beneficial for neuroregeneration (brain-derived neurotrophic factor, and fibroblast growth factors, etc).
Accordingly, fasting-induced activation of autophagy has been proposed to be a promising tool for host defense against SARS-CoV-2 and vaccine-related multiple systemic symptoms, including neurological (brain fog), as well as symptoms caused by dysregulated immune function.
Intermittent fasting restores autophagic flux in islet cells and improves glucose tolerance by enhancing glucose-stimulated insulin secretion, beta cell survival, and pancreatic regeneration via activating the autophagy-lysosome pathway.
A number of intermittent fasting plans can be adapted and modified to best suit the patient’s lifestyle. For timed fasting, begin slowly: start with a 10-hour eating window 5 days a week, and then reduce weekly to reach the goal of an 8-hour eating window 7 days a week.
Intermittent fasting/timed restricted eating needs to be coupled with a diet that consists of “real food,” minimizing the intake of processed foods.
Note that fasting is contraindicated in patients younger than 18 (due to impaired growth), malnourished patients (BMI < 20 kg/m2), and during pregnancy and breastfeeding.
Patients with diabetes, gout, or those with serious underlying medical conditions should consult their primary care physician prior to undertaking to fast, as changes in their medications may be required, and these patients require close monitoring.
It is important to stay well-hydrated during fasting periods; drink lots of water and/or an electrolyte solution.
Intermittent fasting represents a simple, safe, and inexpensive means to benefit people and free them from a variety of symptoms. As Mark Twain (1835–1910) once remarked, “A little starvation can really do more for the average sick man than can the best medicines and the best doctors.”
Sunlight, Near-Infrared Radiation, and Photobiomodulation
Sunlight has great healing powers. Our forefathers roamed the earth and were exposed to sunlight on a daily basis, likely leading to profound health benefits.
During the 1918 influenza pandemic, “open-air treatment” appeared to be the most effective treatment for seriously ill patients. The importance of sunlight and copious amounts of fresh air in self-healing appears to have substantially reduced deaths among patients.
Studies have shown that exposure to sunlight may alleviate multiple conditions, including myocardial infarction, depression, bipolar disorders, premature babies with jaundice, and stress and pain after surgery.
A large prospective study in Swedish melanoma patients has demonstrated that the all-cause mortality rate amongst those who avoid sun exposure was approximately two-fold higher compared to the group with the highest sunlight exposure.
Most people may believe that the main benefits of sunlight come from UV radiation stimulating vitamin D synthesis. However, beyond vitamin D, there are multifactorial and related benefits with photobiomodulation by red and near-infrared light. Red and near-infrared (NIR) radiation have a profound effect on human physiology, notably acting as a mitochondrial stimulant, increasing ATP production.
Amongst all the waves in sunlight, near-infrared radiation (NIR-A) with a spectrum of 750-1500 nanometres has the deepest penetration into tissues, reaching up to 23 centimeters deep.
Furthermore, NIR light increases the production of melatonin in mitochondria, which thus increases autophagy, as described above.
The increased body temperature induced by NIR-A and NIR-B also activates the production of heat shock proteins (which increase autophagy) and essential cell stress survival pathways.
“Yesterday I heard from a patient who was almost completely bedridden due to long COVID. She bought an infrared sauna and says it resurrected her life. She can now work and look after her child,” said Dr. Marik.
Quality and Timely Sleep
There are three main reasons why sleep is important for autophagy.
First, most of our brain-based autophagy happens during the night when we’re in deep sleep. Autophagy has a rhythm just like our human body, and it is optimized when we align our internal rhythm with the sun’s cycle around the earth.
Second, autophagy also happens during sleep because when we sleep, we fast. However, if we eat a big meal right before sleeping, we’re not going to have autophagy.
Third, melatonin secretion increases soon after the onset of darkness. It peaks in the middle of the night, between 2 and 4 a.m., and gradually falls during the second half of the night. As aforementioned, melatonin can also boost autophagy.
Quality and timely sleep are also good for maintaining our natural immunity with the help of two other hormones that sleep helps to boost—growth hormones and endorphins. There are far more secrets behind sleep, which is a topic worthy of being addressed in another paper.
In other words, let us align with the sun’s cycle around the earth. Sleep as the sun sets, awaken as the sun rises, and we’ll be good!
Meditation
Another healthy lifestyle component that can activate autophagy is sitting in meditation.
A study published in the journal Nature–Translational Psychiatry in 2016, followed 64 healthy women, half of whom were given a vacation, while the other half meditated. After one week, it was found that the meditators had significantly lower serum levels of Aβ40, which implies increased autophagy in brain nerve cells and a reduced risk of dementia.
This finding echoes the findings of a study published in the journal Neurobiology of Aging in 2007. The study compared the gray matter volume in the brains of meditators and non-meditators. It was discovered that the gray matter volume of the meditators did not shrink with age, but even increased, suggesting that meditation reverses the aging of, and damage to, the brain.
Meditators also showed great improvement in their ability to concentrate and in their response times, things which may help long COVID patients suffering from brain fog.
Exercise
Studies on the beneficial health effects of exercise have traditionally focused on metabolic boosting, as well as promoting the functions of the respiratory and cardiovascular systems.
However, the potential autophagy-dependent beneficial effects of exercise are also robust. The recycling of cellular components by autophagy is an important factor involved in the beneficial responses to exercise.
Exercise positively regulates the autophagy capacity/flux of skeletal muscle via certain proteins and pathways.
Exercise-induced activation of autophagy in skeletal muscle has been shown to be influenced by transcriptional regulation of autophagy-related genes (ATGs).
The beneficial effects of exercise include the degradation of oxidatively damaged proteins and organelles, improved mitochondrial oxidative capacity, improved glucose regulation, protein synthesis, preservation of muscle strength and mass, and improved endurance exercise performance.
It was observed that treadmill exercise (8 weeks) in mice positively modulated the levels of autophagy-associated proteins, improved autophagy, reduced the number of toxic proteins (alpha-synuclein), and thus boosted neuroprotection.
Other studies have also shown that exercise training boosts autophagy-associated lysosomal pathways and promotes mitochondrial biogenesis in aged hippocampal neurons, indicating the benefit of potentially preventing neurodegenerative conditions and aging.
Patients with long COVID and post-vaccine symptoms frequently suffer from severe post-exertional fatigue with worsened symptoms after exercise. Problems with exercise in COVID-19 patients, particularly with the vaccine injured, have been terribly debilitating.
Therefore, we suggest light movements, such as walking, tai chi, yoga, or relaxation therapy. More robust exercises, such as intense aerobic exercises, may be too taxing.
Natural Molecules Boosting Autophagy
There are also a number of nature-derived molecules that can boost autophagy. Here we will introduce a few of them, including ivermectin, melatonin, resveratrol, spermidine, and terpene nutrients.
Ivermectin
Ivermectin (IVM), originally derived from Japanese soil, is an FDA-approved anti-parasitic drug that has a broad-spectrum antiviral activity and inhibition against the SARS-CoV-2 virus.
In an in vitro cellular model, when ivermectin was added at 2 hours post-SARS-CoV-2 infection, there was a ~5000-fold reduction of viral genetic material at 48 hours.
Ivermectin binds to the spike protein and helps prevent its entry into our cells, reducing the burden of spike protein from the outset.
Furthermore, Ivermectin also induces autophagy through an intracellular signaling pathway named “AKT/mTOR.”
Melatonin
Melatonin is a pleiotropic molecule that not only reduces oxidative and cellular stress but also regulates the immune system and activates the autophagy pathway by reinforcing unfolded protein response (UPR) and unlocking autophagy blockage. This allows autophagosomes to bind to lysosomes, completing the process of autophagy, and decreasing viral replication.
Melatonin is a smart molecule. It differentially modulates autophagy and the related pathways in normal versus tumor trophoblast cells, being cytoprotective in normal cells, whilst increasing apoptosis in tumoral trophoblast cells.
Resveratrol
Resveratrol (RSV) is a natural compound that has recently attracted much attention for its antioxidative effects on multiple diseases. Resveratrol reduces both apoptosis and inflammation. It is distinguished because it regulates several cellular processes that prevent cellular injury and increase viability.
RSV is naturally present in foods such as grapes, blueberries, and peanuts, to name a few.
In addition, resveratrol induces autophagy by inhibiting mTOR through multiple pathways, such as promoting the association between mTOR and DEPTOR, triggering the phosphorylation of Raptor via activating AMPK and directly inhibiting mTOR, and as a SIRT1 activator to active AMPK and directly inhibit mTOR.
As an inducer of autophagy, RSV has multiple beneficial effects in different pathologies, ranging from the energetic regulation of the cell (promoting ATP production) to the regulation of neural regeneration.
Spermidine
Spermidine is a naturally occurring polyamine that, like resveratrol, has anti-inflammatory and antioxidant properties. It preserves mitochondrial function and has been shown to reduce cardiovascular disease and prolong lifespan.
Spermidine plays a central role in cellular homeostasis and self-repairing mechanisms that promote macroautophagy/autophagy via directly inducing phagosome-lysosome fusion, helping induce eIF5a, which in turn, induces genes to start autophagy (ATG3 and TFEB) and improve mitochondrial respiration.
The polyamine pathway is highly conserved from bacteria to mammals.
Spermidine is prominently found in aged cheese, wheat germ, nuts, soybeans, mushrooms, broccoli, apples, and pears.
Terpene Nutrients
In addition to resveratrol and spermidine, there are other health-improving nutrients from plants that can promote autophagy.
In an article published in the journal Aging in 2021, Russian scientists found that terpenes extracted from Siberian fir trees could effectively activate autophagy.
After treating cells with terpenes for 24 hours, the percentage of cells containing autophagosomes (garbage bags) or autophagolysosomes (garbage processing stations) both increased significantly compared to the control group, and the number of autophagosomes contained in a single cell also increased.
Reduce Intake of Acid Blockers
Proton pump inhibitors (PPIs) should be avoided as they prevent the acidification of lysosomes and disrupt the autophagy pathway.
The spike protein has been reported to damage the mitochondrial functions of our epithelial cells, while PPIs also accelerate endothelial senescence. Therefore, PPIs should be used with caution for anyone suffering from long COVID or vaccine-related injuries.
The Human Body’s Potential
The prolonged pandemic has affected the human body in many ways, including putting tremendous stress on our neurological and mental health.
The body has enormous capabilities for self-healing and self-repair. Our approach is to help the body heal itself. There are a number of natural strategies we can employ to help boost our body’s autophagy process.
While different approaches may appear unrelated, they are actually interconnected with one another. A combination of different methods may have synergistic effects, and we may have to find an individualized way of combining these approaches, as each person’s body and the condition is unique.
By taking a holistic approach and understanding the interconnections among our endowed natural healing mechanisms, we may have a better chance of fundamentally improving our physical and mental health.
About the Authors- Dr. Yuhong Dong, a medical doctor who also holds a doctorate in infectious diseases in China, is the chief scientific officer and co-founder of a Swiss biotech company and former senior medical scientific expert for antiviral drug development at Novartis Pharma in Switzerland.
- Dr. Paul Ellis Marik is a medical doctor and professor of medicine. Dr. Marik was Chair of the Division of Pulmonary and Critical Care Medicine at Eastern Virginia Medical School in Norfolk, Virginia. He was the director of the medical ICU at the Norfolk General Hospital, and critical care doctor at Sentara Norfolk General Hospital. Dr. Marik is a co-leader of the Front Line COVID-19 Critical Care Alliance (FLCCC).






.png)

Comments
Post a Comment