Dr Pierre Kory: Hospitalized COVID-19 Patients are Systematically Dying from Under-Treatment with Corticosteroids?
PART 1 - As a now renowned (infamous?) U.S pulmonary & critical care specialist with numerous co-authored publications and extensive experience treating COVID-19 in all it’s phases, almost every day of this pandemic, and sometimes multiple times a day, I am contacted by someone in my ever-widening circle of friends, family, or colleagues asking me to help a loved one who is deteriorating from COVID in the hospital. The case is invariably one of an often older (but not always) patient mired on a hospital ward or in an ICU, whose illness has progressed to the point where they require near maximal or maximal oxygen/ventilator settings and the patients and family members begin to question whether “enough is being done” or “is there more the doctors should be doing?” So they reach out.. desperate for help.
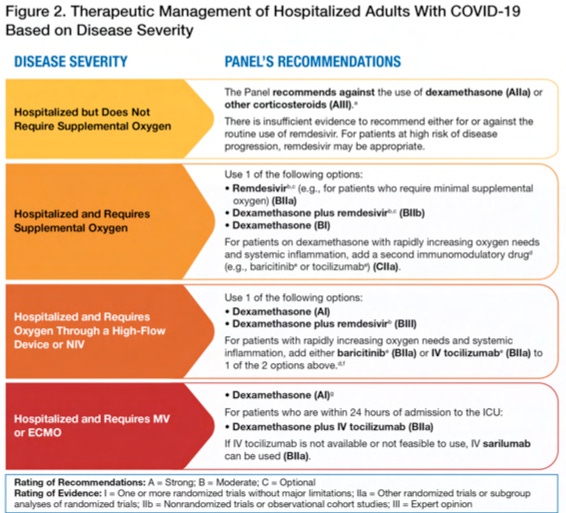
The therapeutic regimen that their loved one is on is nearly identical in almost all cases, especially on the hospital wards where a generally anemic dose of a corticosteroid called dexamethasone (standard of care worldwide for COVID patients in the pulmonary phase of disease), along with remdesivir (“run death is near” as some nurses have called this drug), and occasionally a medicine ending in “ib or ab” (classes of expensive medicines that block a specific inflammatory mediator called a cytokine, such as tocilizumab, sarilumab, or baricitinib) and some form or dose of a blood thinner. If lucky, some may get high-risk, costly interventions such as Vitamin D or zinc or melatonin (sarcasm noted yes?), and patients are generally on or have completed some almost certainly unnecessary antibacterial agent “just to be sure.”
In later posts I might explore some of the above raised issues more deeply, like the corrupt dangers and inefficacy of remdesivir, the costly and needless “ibs and abs”, antibiotic over-use etc. but today, I want to focus on the singular and most important treatment deficit (too low a dose of corticosteroid), which, if systematically corrected, likely presents the greatest opportunity to improve the survival chances of COVID-19 patients after entering the hospital by keeping them out of ICU’s and off ventilators (and reducing the accumulating PTSD I acquire from these daily calls for help). Please note that in almost every single instance that I am asked to help, I can offer zero help because less than 1% of physicians either feel they need outside help or desire to have a clinical discussion with a supposed “expert” (the near majority of docs are convinced they know COVID as much or more than anyone else).
So, I thought it might be interesting to run through the “history” of my own and the Front-Line COVID-19 Critical Care Alliance’s (FLCCC for short) long-standing knowledge of the need for higher dose corticosteroids in COVID-19.
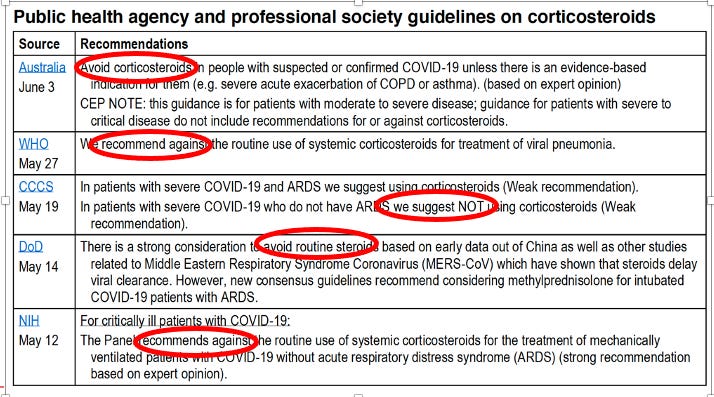
Let’s start at the beginning when COVID-19 began to roll across the world. Every doctor caring for a COVID-19 patient was looking for guidance on how to treat the disease. The below table summarizes the inital guidance they recieved on the use of corticosteroids, coming from the worlds major national and international health care societies:
And so was born the FLCCC’s first mission: advocating for effective treatment of COVID-19 by trying to get the world to understand that it was a “corticosteroid responsive disease.” Off we go:
April 2020 – Dr. Umberto Meduri, one of the founding members of the FLCCC, co-authored a paper with a group of international critical care experts which argued against the global prohibition against corticosteroids in severe COVID-19 acute respiratory distress syndrome (ARDS), based on a robust analysis of studies conducted during prior coronavirus and influenza pandemics (SARS, MERS, H1N1) as well as his deep, lifetime career experience studying the role of corticosteroids in severe lung injuries and critical illness. All the leading health agencies above were echoing a misinterpretation of the observational data from those pandemics in that although those earlier studies found that patients who received corticosteroids died more frequently than those who did not, it was also true that the patients that were more severely ill and more likely to die…were given steroids! Meduri’s group argued that the largest and most carefully done analyses of SARS and H1N1 studies (by carefully controlling for dose, timing, severity of illness, age, and comorbidities found that treatment with corticosteroid therapy in viral induced ARDS.. led to a massive 50% reduction in mortality. Despite the fact that the Society of Critical Care Medicine blasted this paper to many thousands of their members.. the paper and its conclusions was ignored by every society and health care agency across the world (with the exception of the FLCCC :)).
May 2020 - I left the University of Wisconsin to help my former hospital in New York City - Mount Sinai Beth Israel. They were inundated with severe hospital cases and all my former colleagues and trainees were exhausted. Upon resuming the care of my old ICU, I became quickly intrigued by how all these COVID patients were presenting early on with “happy hypoxia” - a description meant to convey the combination of low oxygen levels with a lack of breathlessness or discomfort. I had definitely seen patients present in similar fashions but they were rare in my mind.. I couldn’t put my finger on the connection until one night, I was obsessing about this familiarity as I was trying to fall asleep, when it suddenly hit me that these patients reminded me of patients with a rare-ish disease called “organizing pneumonia (OP).” The name is actually a confusing one becuase OP is not an infectious illness but instead a reaction to a lung injury, typically from an unknown source or most commonly a drug reaction. In some cases, it can be “associated with” or “caused by” a viral infection but it is not a true infection itself.. in that, the treatment is as follows: 1) remove offending agent/drug and/or 2)treat with... corticosteroids (and use high, “pulse doses” in fulminant cases). These patients were notoriously in need of oxygen, often for prolonged periods, and often in high fractions despite being fully conversant and not in overt respiratory distress while resting in their hospital beds. “Happy Hypoxia” solved! SARS-CoV2 was causing an “organizing pneumonia”.. in almost everybody?
So, in order to validate my hypothesis, first thing the next morning, I called my friend and close colleague Dr. Jeff Kanne at the University of Wisconsin, one of the worlds premier chest radiologists and someone whose intelligence and skill in the field is nearly unparalleled. As soon as he answered the phone I said, “Jeff, what would you say if I told you that I think that all of these Covid patients are suffering from organizing pneumonia?” His answer? “Of course it is, we wrote this up in March in the journal Radiology after an expert panel that I chaired had completed our review of all the CT scans from Wuhan.” (turns out they literally had written in their expert report “the most common reported CT findings in COVID-19 patients are typical of an organizing pneumonia pattern of lung injury.” I then started yelling “no clinicians read radiology journals! We need to publish this in a clinical medical journal! Like NOW!”. We quickly agreed to write it up together. I went home after my ICU shift and started working furiously on it. The paper accumulated the radiographic, pathologic, and clinical evidence to try to prove that the pulmonary phase of COVID-19 was an organizing pneumonia and that the first line therapy for this condition was.. corticosteroids. As brilliant as this hypothesis was (forgive me for I am biased) it took me 4 months and 6 journal submissions with 2 peer reviews until it was finally published in a prominent journal. The highlight of that journey was the rejection letter I received after a rigorous peer review in the American journal Chest, when the peer reviewer who voted for rejection wrote, “in order for this paper to be published, a randomized controlled trial of corticosteroids would need to be performed.” Yup.
This paper by founding FLCCC member Dr. Umberto Meduri, a world expert on the use of corticosteroids in critical illness and acute respiratory distress syndrome (ARDS), found that in the best ICU studies of prior viral pandemics, corticosteroids decreased mortality by 50%.
Note that in one of the main studies he referenced, they compared different doses of corticosteroids used in viral ARDS and found that 80mg of methylprednisone daily led to the largest improvements in survival, a dose far higher than the 6mg of dexamethasone the world uses now (that dose is approximately equivalent to 32mg of methylprednisone)
This paper by founding FLCCC member me, which compiled all the evidence that COVID pneumonia is actually a rare-ish diseae called “organizing pneumonia,” (OP) and the gold standard treatment of OP is corticosteroids , and in “fulminant” cases of OP, high, “pulse doses” (i.e. sometimes equaling 1,000mg daily of methylprednisone for 3 days) are recommended.
Note that these two papers were published or being reviewed by journals in the Spring of 2020, a period marked by a widespread prohibition against their use while inexplicably high mortality rates, with frequent prolonged durations of mechanical ventilation (MV) were being reported among multiple early studies of COVID-19-associated acute respiratory failure. These reports were emanating from centers expert in such supportive care strategies. Yet, many of these same centers were literally running out of ventilators and governmental agencies started scrambling and competing to purchase huge lots of them.
In critical care medicine, I am what is known as a “vent geek,” having long ago developed an obsession with setting pressures and flows, initiating weaning , and interpreting waveforms. Further, given I was the Medical Director of the Trauma and Life Support Center at the University of Wisconsin at the time, the State Health Department had me on daily calls helping them evaluate the strengths and weaknesses of the various, often older or more basic ventilators being offered to them by vendors in large numbers.
To get a sense of how bad critical care docs were failing at keeping people off ventilators or successfully liberating them once on, one major heath system in Manhattan went from having 95 ICU beds across their 6 hospitals to 345 ICU beds in the span of two weeks (personal communication with system critical care leadership). This was all occurring in the setting of a widespread “supportive care only” strategy; meaning simple Tylenol, hydration, nutrition, and oxygen. No specific therapies were tried.. which led one major center in the New York City area to publish an 88% mortality for those on ventilators (umm.. 30% ICU mortality is considered very high). But more and more evidence supporting corticosteroids was accumulating..while critical care systems were cratering;
This remarkable study matched the inflammatory gene expression patterns induced by SARS-CoV2 in human lung tissue tissue against a database of the expression of gene suppression changes triggered by over 5,000 FDA-approved drugs.. and found methylprednisolone to be the drug with the greatest potential to revert the changes induced by COVID-19, while other closely related corticosteroids, such as dexamethasone or prednisone, were not. Methylprednisone was #1 out of over 5,000 medications. Also note this type of search for and analysis of existing therapeutics mechanisms of action allows for the rapid identification of optimal therapeutics - a powerhouse approach in a pandemic situation (and avoids the years of delay and billions of dollar needed to develop novel, high-cost, patentable drugs such as the mutagenic molnupiravir that the system is trying to shove down our throats. Just sayin’.
Observational studies reporting large impacts of corticosteroids from Detroit and Italy started to appear on pre-print servers.. and were promptly ignored beause they were not gold-standard randomized controlled trials (fun fact: on average, randomized and observation controlled trials throughout the history of modern evidence based medicine..reach the same conclusions. A known fact proven over decades, yet suppressed and fought against by Pharma who instead prefer Science to rely solely on big Pharma conducted RCT’s to “prove” something works or doesn’t.
Physicians on social media.. started to make noise. Hospitalists and intensivists started posting, largely anonymously, compelling observations and experiences, essentially crying out for doctors to start using corticosteroids at the first sign of low oxygen in COVID patients. Some memorable posts read as follows:
“We floundered for two weeks. Lots of codes, intubations and death. Maybe 15 discharges. We started steroids and discharged 250 patients. Less intubations, less codes. And the ones that ended up on vent, not as serious. CXR/CT Changes = steroids. Hypoxia on admission = steroids. Ambulatory hypoxia = steroids. Completely changed our trajectory Steroids are a game changer.” Hospitalist, SE Michigan - our group is taking care of 700 plus COVID+ patients
“I'm here in New Orleans, since we started using steroids, we were able to free ventilators and get elderly patients out of the hospital without needing a ventilator. Patients that were obviously crashing quickly, who we had to have end of life talk with were able to walk out of the hospital. At no point did any of our patient’s worsen because of steroids. These patients shed viruses 4 weeks later, with or without steroids. The virus doesn't kill anybody, it’s the inflammation that does. Let the virus replicate however slow down the inflammation”
Since this info emanated from social media and was not approved by the agencies or the journals, it pretty much met the definition of what would later be attacked as.. medical misinformation. Or were they instead valuable “reports from the front lines?” Yet the authorities continued on with their damn “supportive care only” approaches. ICU bed numbers continued to swell.. and people died. A lot. Often after weeks of being in hospital or ICU, lonely, not able to see family. Unforgettable.
I/we in the FLCCC got lucky when I was invited to testify in the U.S Senate by the Senator from Wisconsin, Ron Johnson, who chaired the Senate Committee on Homeland Security & Governmental Affairs. He decided to hold hearings as to why, in my words (and likely his too) “the doctors were not doctoring” and U.S citizens were effectively being denied treatments or attempts at treatment. Spot on really. I got the invitation because he had found the FLCCC website and protocols and noticed that one of the founders was from Wisconsin so I immediately received a phone call and invitation. Watching it again, a year and half later, I was struck about how much we knew back then about how to treat the disease and how strongly we made the argument for corticosteroids. Months before all the randomized trials (RCT). Further, I must point out that I every element of our protocols was incorporated many months before later having been proven in an RCT. With corticosteroids, it was not until late June 2020, when a press release announced from across the pond, that Oxford University’s RECOVERY trial, testing 6mg of dexamethasone daily, had found a small, but statistically significant reduction in mortality when used in patients on oxygen and an even larger one in patients on mechanical ventilation.
The only question that remains is.. what else have we learned about corticosteroid type, dose, or duration since the Oxford study in June of 2020? Turns out.. a lot. Check out this table I made below, and look at the column “number needed to treat (NNT)" to save a life.” The NNT is one of the most valuable measures in medicine as it indicates the potency or impact of a medicine on a certain outcome. Note that the lower the number, the higher the impact. And you can see, that higher doses, especially of methylprednisone (shocker) are FAR superior than using 6mg of dexamethasone. Over and over, by comparing studies side by side, or head to head (bottom rows), methylprednisone, at higher doses, consistently leads to many more lives saved. Especially when started early in the hospital.
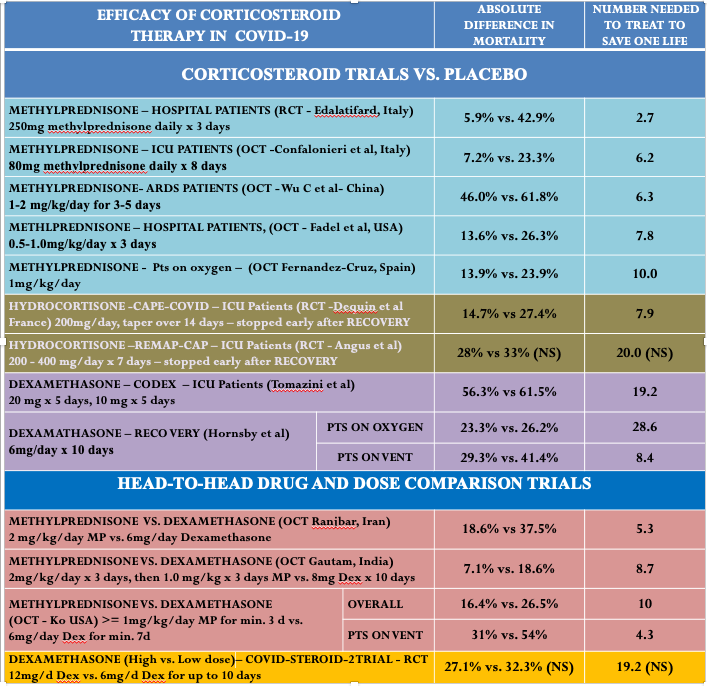
The trial from Iran by Edalitifard (first row) is by far the most impressive. They gave 250mg of methylprednisone for three days to patients in the “early pulmonary phase,” before they required intubation and mechanical ventilation. They reported a massive mortality benefit with an NNT of 2.7. Meaning that for every three patients you treated with that dose and drug, one life would be saved compared to if you had not done so. This is a massive effect in medicine. Of note, when you perform electrical defibrillation of a patient dying from a malignant arrhythmia like ventricular fibrillation, that has an NNT to save a life of… 2.5. So, giving a COVID patient early “pulses” of 250 mg of methylprednisone is akin to defibrillating someone out of a life-threatening ventricular arrhythmia? Wow. Yet the world continues giving 6mg of dexamethasone daily.. which has an NNT somewhere between 8-29.
As an intensivist who has known this data for over a year, has worked in ICU’s in 5 different hospitals around the country, has repeatedly begged my hospitalist colleagues (the docs caring for the patients before they crash into ICU’s) to be more aggressive with corticosteroids so as to avoid deterioration and needless death, I have rarely succeeded in getting my colleagues to change their corticosteroid dosing practices (they are seemingly all waiting for this recommendation to be incorporated into a guideline handed down from the “gods of science and knowledge” in Washington). Unreal..except it’s not. I have been watching needless death all around for so long… I am almost used to it. Almost.






.png)

Comments
Post a Comment