POTS and COVID: Blue Legs, A New Long-COVID Symptom; How to Test for and Treat It
It started with an uncomfortable tingling and itchiness in his legs after standing for 10 minutes. Then, the he watched as his lower limbs turned blue right before his eyes. He was experiencing acrocyanosis, a pooling of blood in the extremities that had never afflicted him before.
Doctors attributed the 33-year-old man’s symptoms, which started 18 months prior, to a bout of COVID-19 he had suffered then, according to a recent case study in The Lancet. His case provides new evidence that the virus may cause lasting dysautonomia—dysfunction of the autonomic nervous system—that experts are only beginning to understand.
“This was a striking case of acrocyanosis in a patient who had not experienced it before his COVID-19 infection,” Dr. Manoj Sivan, associate clinical professor and honorary consultant in rehabilitation medicine at the University of Leeds’ School of Medicine, said in a press statement.
POTS and Long COVID
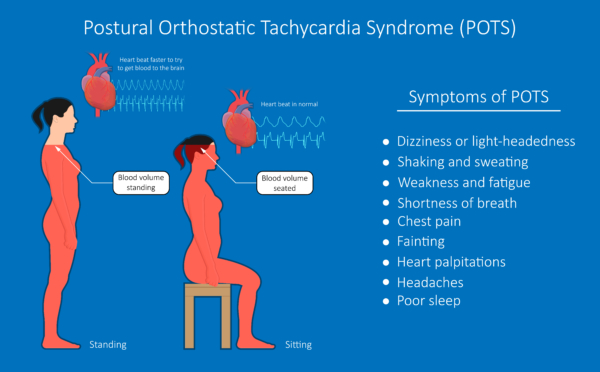
The anonymous patient had already been diagnosed with postural orthostatic tachycardia syndrome (POTS)—a form of dysautonomia for which reddish-blue discoloration of the legs can be a symptom—two months earlier by a cardiologist. POTS is a blood circulation disorder that causes an abnormal increase in heart rate when transitioning from sitting or lying down to standing up, which can also lead to lightheadedness, fainting, and fatigue.
POTS is a relatively uncommon condition, affecting an estimated 500,000 to 1 million people in the United States. It is most commonly diagnosed in women between 15 and 50 but can occur in people of any age and sex.While the exact cause of POTS in long-COVID patients is unclear, it may be related to the virus’ impact on the autonomic nervous system. SARS-CoV-2, the virus that causes COVID-19, has been found to directly affect the nervous system, causing inflammation and damage to the nerves that regulate heart rate, blood pressure, and other autonomic functions.
There is no known cure for POTS, but doctors may prescribe medications to help manage symptoms, such as beta blockers, fludrocortisone, and midodrine.
“Patients experiencing this may not be aware that it can be a symptom of long COVID and dysautonomia and may feel concerned about what they are seeing,” Dr. Sivan added, noting that doctors themselves may be unaware of the link between long COVID and acrocyanosis.
Nearly 2 in 3 People With Long COVID Experience Autonomic Dysfunction
About 28 percent of people infected with COVID-19 develop long-COVID symptoms, according to a survey by the KFF, formerly known as the Kaiser Family Foundation, a health policy research organization. For the majority, the symptoms clear up, but 11 percent are left with persistent long COVID.
A separate online survey of over 2,300 adults with long COVID found that 67 percent had moderate to severe autonomic nervous system dysfunction. This was unrelated to the severity of their initial COVID-19 illness, suggesting autonomic dysfunction is highly prevalent in long-COVID patients. This may be due to COVID-19’s effect on a vital part of the nervous system.
“Extensive research has shown that long COVID causes malfunction of the key almond-size circuit breaker in the brain called the hypothalamus,” Dr. Jacob Teitelbaum, a board-certified internist and nationally known expert in the fields of chronic fatigue syndrome, fibromyalgia, sleep, and pain, told The Epoch Times. The hypothalamus not only controls the autonomic nervous system functions but also sleep and hormone regulation.
Without treatment, there is a risk autonomic dysfunction can become progressive, Dr. Teitelbaum said. “Other key parts of the autonomic nervous system can begin to fail along with the hypothalamus,” he added. “These include, especially, the vagus nerve and the nerve fibers that control blood vessels. The latter is called small fiber neuropathy.”
How to Screen for and Treat POTS at Home
Dr. Teitelbaum described a simple at-home test to check for symptoms of POTS.
First, lie down for 10 minutes and check your pulse rate. Then, stand up in one place for 10 minutes, without leaning on anything, while checking your pulse every two minutes.
If your pulse rate rises by 20 beats per minute or more during the 10 minutes of standing, it indicates orthostatic intolerance, he said.
“However, if your pulse rate goes up by 30 bpm or more, [the test] confirms [POTS].”
If signs of POTS are detected, Dr. Teitelbaum recommends self-care approaches to relieve symptoms. Treatment for POTS in long-COVID patients is similar to treatment for non-COVID POTS cases, typically involving lifestyle changes and medications.
Helpful lifestyle changes can include moderate physical activity and avoiding triggers that worsen symptoms. Wearing medium compression stockings when up and around, along with increased salt and water intake, are simple at-home treatments, according to Dr. Teitelbaum.
“Knee-high compression stockings can help, but thigh-high ones are better,” he added.
A study published in the Journal of the American College of Cardiology (JACC) in 2021 indicated that consuming a slightly higher amount of salt can lower plasma norepinephrine levels, reduce heart rate variability, and improve clinical symptoms.
Diet and nutrition are other crucial aspects for improving POTS. Doctors advise developing the following habits:
- Increase daily sodium intake from 3,000 milligrams to 10,000 milligrams.
- Consume 2 to 2.5 liters of water per day.
- Opt for frequent and smaller meals.
- Follow a diet rich in fiber and complex carbohydrates to help reduce blood sugar spikes and alleviate symptoms.
- Maintain nutritional balance with protein, vegetables, dairy products, and fruits.
- Opt for salty snacks such as broth, pickles, sardines, olives, anchovies, and nuts. Choose healthier options and avoid relying on chips and crackers for salt intake.






.png)

Comments
Post a Comment