New Study Questions the Validity of Long-COVID
Long-COVID
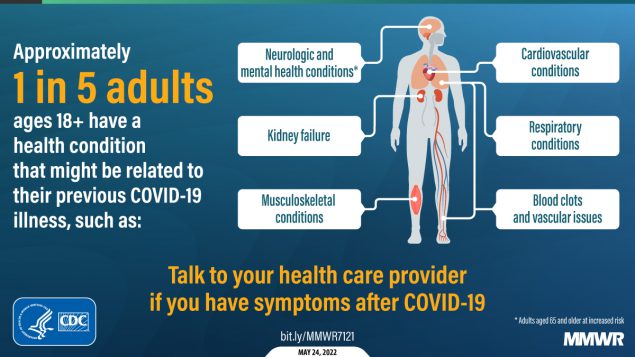
The idea behind long-COVID is that symptoms continue long past the time that the patient has mostly recovered from the SARS-Cov-2 virus. The most common symptoms include fatigue, shortness of breath, muscle pain, joint pain, headache, cough, chest pain, altered sense of smell, altered taste, and diarrhea (1). The problem is that outside of the loss of the sense of smell, all of these symptoms can be caused by hundreds of different medical conditions. In addition, while severe post-COVID ARDS is quite real and can ruin lives, long COVID lives in a different category of general malaise.
The US Department of Health and Human Services has estimated that as many as 23 million Americans have long-COVID (2). CNBC this week estimated that long COVID would cost the American economy 3.7 trillion US dollars, an amount rivaling the economic impact of the great recession.
Long COVID has also been a boon to functional medicine practices around the world as these patients often get no answers from traditional doctors. I have personally seen dozens of patients that are convinced that COVID-19 caused everything from craniocervical instability to their back pain. Surprisingly, even major universities have jumped into the fray. For example, institutions like Stanford, Mayo, and Harvard have all opened long COVID clinics. This last move surprised me, as while the functional medicine community has long been known for lack of scientific rigor, seeing elite medical schools open clinics before we had definitive research on the veracity of long COVID was a surprise.
What if long COVID wasn’t real? That’s what some new research suggests.
The New Research
The authors from various US medical schools looked at 1,000 US adults who were all seeking care for illness-related symptoms during the pandemic who were both COVID-19 positive and negative (4). They expected to see much more in the way of lingering symptoms 3-months after a COVID-19 infection, which would have supported the idea that long COVID was real. Instead, they observed that 39.6% of COVID-19–positive and 53.5% of COVID-19–negative patients reported residual symptoms and life impacts. Meaning more people who didn’t have COVID-19 and who had a respiratory-type illness had long-term reports of poor physical function, anxiety, depression, fatigue, poor social participation, sleep disturbance, and pain interference.
What does this mean? Feeling unwell 3 months after a respiratory illness was common during the pandemic and COVID-19-positive patients felt generally better at 3 months than those who never had the illness. The authors posited that it was likely the other effects of the pandemic like social isolation, anxiety about the future, and an overall sense of impending doom that was causing long COVID symptoms and not the virus itself. From the article:
“The presence and persistence of poor mental health among nearly 1 in 4 participants (21.9% of the COVID-19–positive group and 27.3% of the COVID-19–negative group) may reflect a more general pandemic exposure, which participants in both groups experienced.”
Are We Now Beginning to See Some Academic Rigor Applied to Long COVID?
The biggest problem with Long COVID research to date has been it all assumes that people who present with symptoms after COVID have a unique disease related to the SARS-Cov-2 virus. The problem with descriptive studies that make that assumption is that nobody has yet asked the most basic questions. For example, what specifically defines Long COVID, and what proof is there that these symptoms are related to the SARS-Cov-2 virus? What is the mechanism of action that explains how the virus causes these problems? When this research team asked one of those basic questions, they found out that these symptoms are not unique to those who had COVID and more likely are a response to the conditions of the pandemic and NOT the virus.
The problem is that in a short time, long COVID as a diagnosis has become ingrained in both the functional medicine community and in the US medical schools that opened clinics to serve this patient population. There are now dozens of studies using all sorts of pharma interventions on this patient population. All of this happened before anybody asked the most basic question: are these symptoms caused by the virus or are they caused by the pandemic itself?
The upshot? This study marks a major blow to the idea that long COVID is caused by the SARS-Cov-2 virus. Despite that, it had very little media coverage. The big coverage was reserved for the studies showing that Long COVID would cost us trillions and would be the next big public health emergency. This study suggests the next public health emergency is likely not caused by the virus, but perhaps by our response to the virus.
______________________________________________________
(1) Subramanian, A., Nirantharakumar, K., Hughes, S. et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med 28, 1706–1714 (2022). https://doi.org/10.1038/s41591-022-01909-w
(2) US Department of Health and Human Services. health+ Long COVID. https://www.hhs.gov/sites/default/files/healthplus-long-covid-report.pdf Accessed 12/3/22
(3) CNBC. Long Covid may be ‘the next public health disaster’ — with a $3.7 trillion economic impact rivaling the Great Recession. https://www.cnbc.com/2022/11/30/why-long-covid-could-be-the-next-public-health-disaster.html Accessed 12/3/22
(4) Wisk LE, Gottlieb MA, Spatz ES, et al. Association of Initial SARS-CoV-2 Test Positivity With Patient-Reported Well-being 3 Months After a Symptomatic Illness. JAMA Netw Open. 2022;5(12):e2244486. doi:10.1001/jamanetworkopen.2022.44486
About the Author: Chris Centeno, MD is a specialist in regenerative medicine and the new field of Interventional Orthopedics. Centeno pioneered orthopedic stem cell procedures in 2005 and is responsible for a large amount of the published research on stem cell use for orthopedic applications.






.png)

Comments
Post a Comment