COVID Variant BQ.1.1: What You Need to Know
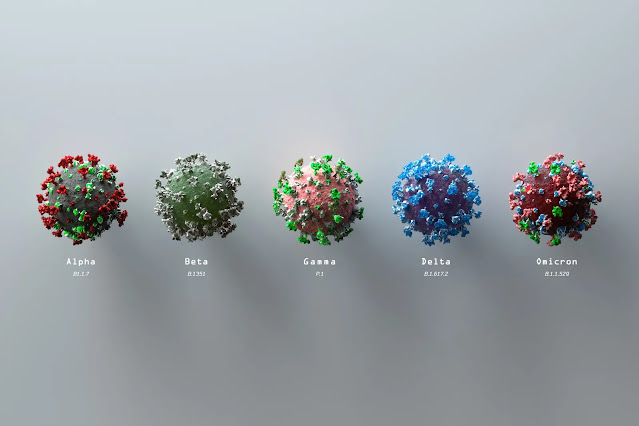
BQ.1.1 is a new Omicron subvariant descended from Omicron BA.5. BQ.1.1, along with its sister variant BQ.1, accounts for around 62.8% of new COVID-19 cases in the U.S. (CDC).
Are BQ.1 and BQ.1.1 More Invasive?
BQ.1 and BQ.1.1 both originate from the same lineage as BA.5. But these new variants may be better at evading immunity than BA.5 due to mutations in the spike protein.So far, the new variants don’t seem to cause more severe infection than earlier Omicron variants. BQ.1 and BQ.1.1 together account for about 60% of the COVID-19 cases in the region including New York and New Jersey—more than any other part of the country (R). But hospitals there haven’t seen a parallel influx in hospitalizations (R).
COVID-19 Omicron BQ1 Variant Symptoms
As of right now, BQ.1 and BQ.1.1 do not seem to have symptoms that distinguish them from previous COVID-19 variants, says William Schaffner, M.D., infectious disease specialist and professor at the Vanderbilt University School of Medicine. “So far, they don’t seem to produce more severe disease, although it’s early,” he says. “There’s nothing distinctive about their symptoms that would tell you that you have one variant over another.”
Possible symptoms include:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Will Current Treatments Work Against BQ.1.1?
One of the most concerning aspects of this surge that treatments like monoclonal antibodies may not stand up to the new variants. Early evidence indicates that due to mutations in the spike protein of BQ.1 and BQ.1.1, Evusheld and bebtelovimab each lose efficacy against the variants, according to the National Institutes of Health (NIH).A combined team of researchers from Leibniz Institute for Primate Research and Friedrich-Alexander University of Erlangen-Nürnberg, both in Germany, has found that the SARS-CoV-2 omicron variant BQ.1.1 is resistant to all known monoclonal antibody treatments. In their study, published in The Lancet—Infectious Diseases (Nov 2022), the group tested a host of omicron sublineages against all known antibody treatments.
In their work, the researchers looked at BJ.1, BA.4.6, BA.2.75.2 and BQ.1.1—all subvariants of the omicron strain of the SARS-CoV-2 virus. They tested each against all of the currently available monoclonal antibody treatments to see how well the treatments are working. They found that all of the variants were resistant to some of the treatments and that BQ.1.1 was resistant to all of them.
This was confirmed by another study, published in the New England Journal of Medicine (Dec 2022).
According to the authors:
"...These results suggest that imdevimab–casirivimab, tixagevimab–cilgavimab, sotrovimab, and bebtelovimab may not be effective against BQ.1.1 or XBB in the clinical setting...These results suggest that remdesivir, molnupiravir, and nirmatrelvir are efficacious against both BQ.1.1 and XBB in vitro..."
Unlike monoclonal antibodies, the antiviral treatment Paxlovid debilitates the virus without needing to fit the virus’ spike protein. That means it should hold up against BQ,1.1, despite its mutations, the NIH said.
Other At-Home Treatments
You can find a listing of doctors who can prescribe necessary home isolation medications on Find a Provider post.
There are many COVID-19 treatment protocols out there on the internet. We have reviewed many protocols and believe the FLCCC I-CARE protocol is the easiest and effective to follow.
Always consult your trusted medical professional before you take any medication or supplement.
Emergency warning signs
- Difficulty breathing
- Persistent pain or pressure in the chest
- Bluish lips or face
- New confusion or inability to arouse
Key Takeaway
As soon as you have symptoms, consult your healthcare provider and start treatment as early as possible. If treatment is delayed i.e. after 5 days of symptoms, your chances of severe COVID are higher.






.png)

Comments
Post a Comment