Link between coronavirus vaccines and Long Covid–like illness starts to gain acceptance
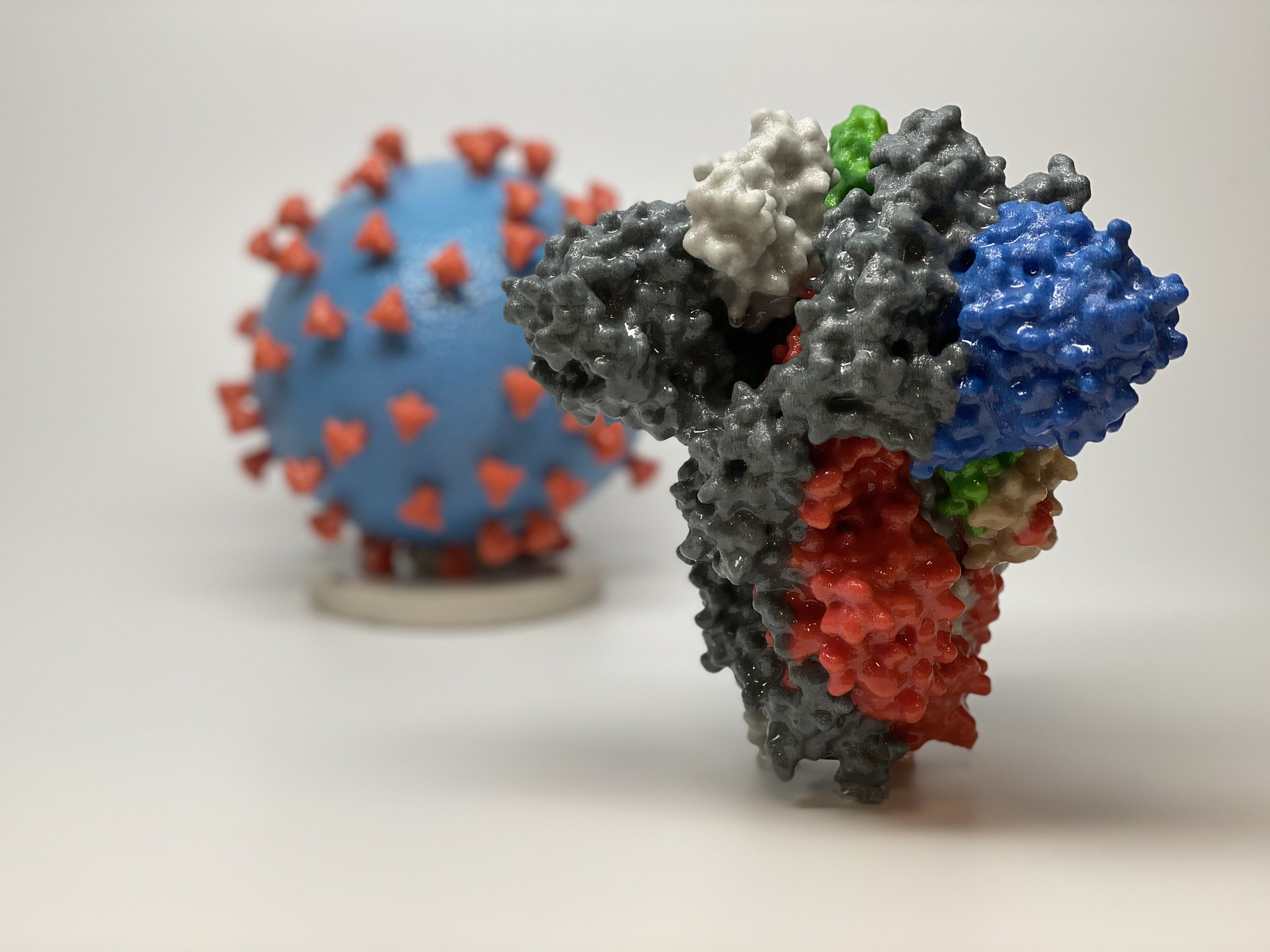 |
| This image shows a 3D print of a spike protein of SARS-CoV-2—the virus that causes COVID-19—in front of a 3D print of a SARS-CoV-2 virus particle. (Courtesy of NIAID/RML) |
“You see one or two patients and you wonder if it’s a coincidence,” says Anne Louise Oaklander, a neurologist and researcher at Harvard Medical School. “But by the time you’ve seen 10, 20,” she continues, trailing off. “Where there’s smoke, there’s fire.”
Cases seem very rare—far less common than Long Covid after infection. Symptoms can include persistent headaches, severe fatigue, and abnormal heart rate and blood pressure. They appear hours, days, or weeks after vaccination and are difficult to study. But researchers and clinicians are increasingly finding some alignment with known medical conditions. One is small fiber neuropathy, a condition Oaklander studies, in which nerve damage can cause tingling or electric shock–like sensations, burning pain, and blood circulation problems. The second is a more nebulous syndrome, with symptoms sometimes triggered by small fiber neuropathy, called postural orthostatic tachycardia syndrome (POTS). It can involve muscle weakness, swings in heart rate and blood pressure, fatigue, and brain fog.
Patients with postvaccination symptoms may have features of one or both conditions, even if they don’t meet the criteria for a diagnosis. Both are also common in patients with Long Covid, where they’re often attributed to an immune overreaction.
Although more researchers are now taking Long Vax seriously, regulators in the United States and Europe say they have looked for, but have not found, a connection between COVID-19 vaccines and small fiber neuropathy or POTS. “We can’t rule out rare cases,” says Peter Marks, director of the U.S. Food and Drug Administration’s Center for Biologics Evaluation and Research, which oversees vaccines. “If a provider has somebody in front of them, they may want to take seriously the concept [of] a vaccine side effect,” he says. But Marks also worries about “the sensational headline” that could mislead the public, and he emphasizes that vaccine benefits far outweigh any risks.
Despite the uncertainties, German Minister of Health Karl Lauterbach acknowledged in March that though rare, Long Covid–like symptoms after vaccination are a real phenomenon. He said his ministry was working to organize funding for studies, although none has been announced so far.
Researchers studying these complications also worry about undermining trust in COVID-19 vaccines. Harlan Krumholz, a cardiologist at Yale University, says concern that the antivaccine movement would seize on any research findings made him hesitant at first to dive in. But about a year ago he and Yale immunologist Akiko Iwasaki began to welcome postvaccination patients into a new study called LISTEN that also includes Long Covid patients. Among other things, it aims to correlate symptoms with immune cell patterns in blood samples.
“I’m persuaded that there’s something going on” with these side effects, Krumholz says. “It’s my obligation, if I truly am a scientist, to have an open mind and learn if there’s something that can be done.”
SCIENCE FIRST wrote about these health concerns in January 2022, describing efforts by scientists at the National Institutes of Health to study and treat affected individuals. A study including 23 people was posted as a preprint in May 2022 but never published. Following Science’s story, almost 200 people contacted the journal sharing their postvaccination symptoms.
Research has since proceeded slowly. This is “a challenging outcome to monitor,” Tom Shimabukuro of the U.S. Centers for Disease Control and Prevention told a government advisory committee in January. Still, more than two dozen case studies have accumulated describing POTS or small fiber neuropathy following a COVID-19 shot, regardless of the vaccine manufacturer.
In 2021, Sujana Reddy, now an internal medicine resident physician at East Alabama Health, published a case study of postvaccine POTS in a 42-year-old man. She then heard from more than 250 people describing similar health concerns. Reddy began a study documenting POTS cases, not yet published, which now includes 55 people who developed symptoms 1 to 2 weeks after vaccination.
Another team scanned for postvaccine POTS across a specific population. Researchers led by cardiologists Alan Kwan and Susan Cheng at Cedars-Sinai Medical Center analyzed a health database of almost 285,000 people in the Los Angeles area; all had received at least one COVID-19 shot. They found that within 90 days after a shot, the rate of POTS-related symptoms was about 33% higher than in the 3 months before; 2581 people were diagnosed with POTS-related symptoms after vaccination, compared with 1945 beforehand. However, the study found a bigger effect from COVID-19 itself: The rate of POTS symptoms in about 12,000 unvaccinated people after infection was 52% higher than beforehand. Although Kwan cautions against extrapolating these numbers to a wider population, he says the pattern is intriguing. “Our data show a relatively clear signal that there probably is an increase in POTS after vaccination and after infection,” he says.
Others find the study compelling. “Even last year I was a little bit cautious” about the link between POTS and vaccination, says Tae Chung, a neuromuscular physiatrist who runs the POTS clinic at Johns Hopkins University. “I didn’t have quantitative data to back it up, but now I feel like I do.” Still, Chung stresses that this paper and other data also suggest COVID-19 vaccines protect against POTS and other Long Covid symptoms, and he remains a strong advocate for vaccination.
AN IMMUNE OVERREACTION to SARS-CoV-2 spike protein, which COVID-19 vaccines use to induce protective antibodies, is one possible cause of these symptoms. One theory is that after vaccination some people generate another round of antibodies targeting the first. Those antibodies could function somewhat like spike itself: Spike targets a cell surface protein called the angiotensin-converting enzyme 2 (ACE2) receptor, enabling the virus to enter cells. The rogue antibodies might also bind to ACE2, which helps regulate blood pressure and heart rate, says Bernhard Schieffer, a cardiologist at the University of Marburg. If those antibodies disrupt ACE2 signaling, that could cause the racing heart rates and blood pressure swings seen in POTS.
Small fiber neurons also have the ACE2 receptor on their surface, so in theory rogue antibodies could contribute to neuropathy. But Matthew Schelke, a neurologist at Columbia University who has treated small fiber neuropathy in both Long Covid and postvaccine patients, says pinning down a connection won’t be easy. Even when unusual antibodies turn up in someone’s blood, “it’s extremely difficult to know if any of these are pathogenic or if they are just bystanders,” he says. Other immune system components that fuel inflammation may also harm nerves, he notes.
Some people appear susceptible to complications after both infection and vaccination, a double vulnerability that can put them in an agonizing situation—eschewing more vaccine doses, often on the advice of their doctors, but also fearing the hazards of Long Covid. Reddy falls into this category. She caught the virus in early 2020 while caring for an infected patient and developed Long Covid, including POTS. Her symptoms dramatically worsened after her first vaccine dose.
An emergency medicine physician in New York City, Saleena Subaiya, experienced the same phenomenon in reverse. Within 24 hours of the second dose of COVID-19 vaccine in January 2021, they developed severe cognitive impairment, fatigue, and a loss of balance. Subaiya improved somewhat over the next year, but was forced to switch to a part-time research job. Then in December 2021, they were hit by Omicron and relapsed.
Postvaccination illness is “a long, relentless disease,” says Lawrence Purpura, an infectious disease specialist at Columbia University who is also Subaiya’s partner—and who treats both Long Covid patients and those with chronic symptoms after vaccination.
A DIAGNOSIS OF POTS or small fiber neuropathy post-vaccination can guide treatment. In POTS, doctors focus on increasing salt and fluid intake to boost blood volume and maintain blood pressure. Beta blockers, which slow racing hearts, may also help.
Small fiber neuropathy is treated with various medications to manage symptoms, and for severe cases sometimes intravenous immunoglobulin (IVIG), an expensive and hard-to-access antibody mixture that can tamp down immune overreactions. Some case studies report that IVIG helped people with postvaccine small fiber neuropathy, at least temporarily.
A more radical approach is plasma exchange, which is sometimes used for autoimmune disorders. Here the patient’s plasma—the liquid part of the blood containing antibodies and proteins—is separated from the blood cells and discarded. The blood cells are then returned to the patient along with a replacement liquid.
Plasma exchange helped a man who developed small fiber neuropathy following his second dose of a COVID-19 vaccine, Schelke and colleagues reported in October 2022 in Muscle & Nerve. “He responded very well,” with months of improvement, Schelke says, but recently returned with worsening symptoms.
Schieffer, meanwhile, has developed an experimental treatment regime that he says showed promise in an unpublished study of eight Long Covid and eight postvaccine patients. It includes statins, which can blunt inflammation in the circulatory system; and angiotensin II type 1 receptor blockers, which can help block the ACE2 pathway activation that may be dysregulated in patients. Schieffer and colleagues are hoping to start a clinical trial of the therapies with 500 people who have either Long Covid or postvaccine symptoms.
Patient advocates are trying to spur new studies. In the next few months, the nonprofit REACT19 plans to distribute small grants, in the tens of thousands of dollars, to teams studying immunology, biomarkers, and other features of postvaccine illness.
Even modest support matters, Krumholz says, because “it’s incumbent on us to produce preliminary data” to win over funders with deep pockets. His and Iwasaki’s LISTEN project now has about 2000 participants, roughly 1000 with Long Covid and 750 with postvaccination symptoms, he says. (LISTEN also includes healthy controls.) He hopes to begin to release results later this summer.
As countries draft plans for a round of updated vaccines, some scientists theorize, reassuringly, that people whose immune systems accepted a previous shot without incident would be highly unlikely to experience immune dysfunction following a booster. But that doesn’t change the urgent need to help those suffering now, Reddy says. “We need to figure out why it’s happening to this subset of people. Why is it happening to them and not everyone else?”
Source:
A version of this story appeared in Science, 2023, Vol 381, Issue 6653. doi: 10.1126/science.adj5565
Myocarditis Not Recovered in 80 Percent at 6 Months After Vaccination




.png)



Comments
Post a Comment