Rise of POTS (postural orthostatic tachycardia syndrome) in the COVID-19 and Vaccine Era
The COVID-19 pandemic casts a concerning shadow in the form of postural orthostatic tachycardia syndrome (POTS). This perplexing health issue, marked by a significant surge in heart rate when standing, is gaining increasing attention in the medical community because of a rise in cases.
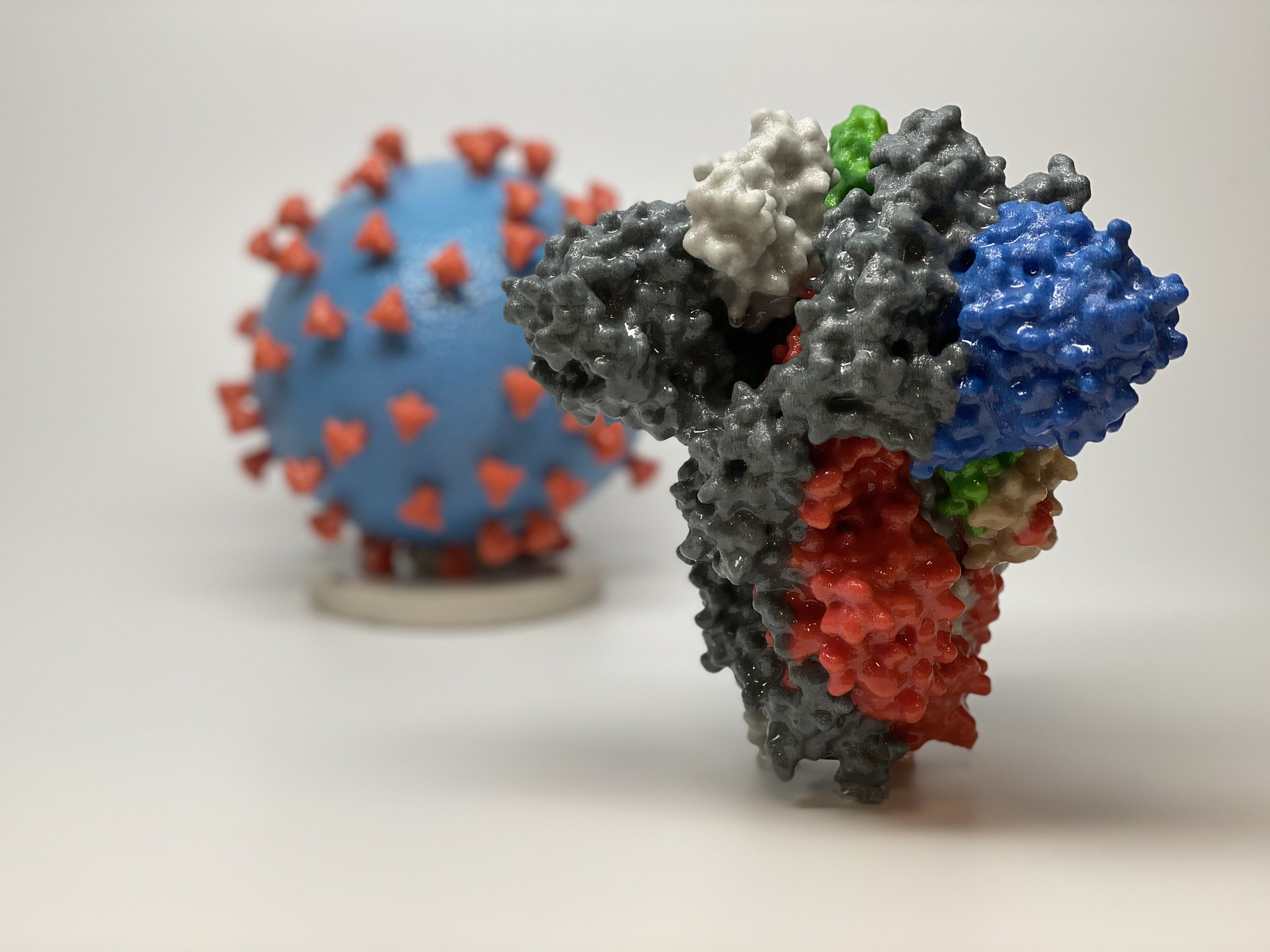 |
| This image shows a 3D print of a spike protein of SARS-CoV-2—the virus that causes COVID-19—in front of a 3D print of a SARS-CoV-2 virus particle. (Courtesy of NIAID/RML) |
2 Journeys, 1 Diagnosis
Phoebe Eaton and Aubrey George, two active women in their mid-20s, found their lives abruptly disrupted by the puzzling symptoms of POTS.
Ms. Eaton, a 25-year-old teacher in training, noted the onset of symptoms after her initial COVID-19 vaccine. She reported recurring urinary tract infections, persistent fatigue, migraines, weight loss, and erratic blood sugar levels. Her health deteriorated after her final vaccine dose.
“I started passing out, which developed into seizures, forcing me to abandon my teacher training,” she said.
For Ms. George, her symptoms surfaced after enduring three concussions within six months. Chronic headaches, dizziness, and fatigue became her unwelcome constants.
Previously dubbed the “Energizer Bunny,” Ms. George now grapples with many symptoms spanning the cardiovascular and digestive systems.
“Every single activity requires extra thought and preparation, which can be exhausting,” Ms. George said.
POTS poses a unique challenge as it’s frequently overlooked.
“Lots of people say to me, ‘but you look so well,’ which is nice to hear, but when you feel rubbish, it makes you feel like you’re lying or making it up,” Ms. Eaton said.
Unmasking the Hidden Disorder Called POTS
POTS falls within the wider category of disorders called dysautonomia. It signifies a malfunction in the autonomic nervous system, which quietly controls crucial functions such as breathing, digestion, and heart rate. When this system falters, as in POTS, it can undermine health and daily quality of life.
POTS primarily manifests as a substantial increase in heart rate when moving from a sitting or lying position to standing. It’s typically diagnosed when a person’s heart rate rises by more than 30 beats per minute within just 10 minutes of standing. For instance, if someone’s heart rate jumps from 70 while seated to 100 or more upon standing, it’s a strong indication of POTS.
For children and adolescents, the diagnostic threshold is higher, requiring an increase of 40 beats per minute or more. The ramped-up heart rate doesn’t coincide with a drop in blood pressure.
POTS presents a wide array of symptoms, including fatigue, headaches, lightheadedness, heart palpitations, nausea, and cognitive disturbances such as brain fog. The mix and intensity of these symptoms, which must be present for at least three months, can fluctuate significantly among patients.
Historically, POTS has been viewed as a rare disorder. Dysautonomia International, a key nonprofit organization dedicated to dysautonomia research and awareness, estimates that POTS affects about 6 million Americans. This number has doubled since the COVID-19 pandemic began, they reported. However, due to the elusive nature of the disease and limited awareness in the health care community, the actual prevalence may be significantly higher.
The variability of POTS symptoms is matched only by their impact on patients’ daily lives. While some individuals with mild symptoms manage to keep up with their regular work, school, and social activities, others may find routine tasks such as bathing, housework, eating, sitting upright, and even standing or walking significantly challenging because of severe symptoms.
“I can’t drive. I tire very quickly and have heart pain and lack of breath when carrying out tasks. I can’t do simple things like emptying the shopping or the dishwasher without passing out. I have lost most of my independence.” Ms. Eaton said.
Specialists treating POTS often compare the functional impairment observed in these patients to those with conditions such as cancer or congestive heart failure.
A pivotal study with more than 5,500 participants has uncovered the economic and employment impacts of living with POTS.
The research, which was carried out in collaboration with Dysautonomia International, revealed that only 48 percent of POTS patients were employed. Among them, 67 percent desired to work more hours but were hindered by their condition.
Nearly three-quarters of participants reported income loss attributed to POTS, with one-third losing more than $10,000 in the year preceding the survey. The research also highlighted broader societal effects, as 28.5 percent of caregivers suffered income loss because of their caretaking duties.
The authors said, “POTS poses a significant risk for reduced employment and increased economic loss in individuals with this disorder and their caregivers.”
Dr. Tae Chung, who leads the POTS program at Johns Hopkins University School of Medicine, observes the stark reality of these statistics in his clinic daily.
“Many POTS patients who remain employed have to modify their lifestyle due to their symptoms,” he told The Epoch Times. “For example, a significant number manage to retain their full-time roles primarily because they are afforded the flexibility to work remotely. This condition hits young people particularly hard, as they often have to work to keep their medical insurance.”
Drawing from his frontline experience, Dr. Chung emphasized the critical situation.
“For these reasons, there’s a pressing need to develop disease-modifying treatment for POTS, alongside improved recognition, diagnosis, and treatment,” he said.
COVID-19 and the Unexpected POTS Increase
POTS continues to pose challenging questions, with a clear-cut cause still eluding scientists. However, the scientific community is increasingly uncovering connections to COVID-19 and its associated vaccines.
While the precise cause of post-COVID POTS is still under scrutiny, potential theories include the production of autoantibodies, direct toxic effects from the virus, or a stimulated sympathetic nervous system response.
“There has been a significant increase in referrals to our POTS clinic since the COVID pandemic,” Dr. Chung said.
He suggested that COVID-19 may predispose individuals to POTS, a theory that he says is supported by emerging research.
Echoing this, Dr. Jordan Pastorek, supervising physician at The POTS Treatment Center, has observed this shift.
“A significantly large portion of our patients now report their POTS symptoms starting after a COVID infection or a dose of the vaccine. This is a noticeable shift from pre-pandemic times when we commonly saw POTS cases resulting from infections like influenza, Lyme disease, and mononucleosis, as well as concussions,” Dr. Pastorek said.
His insights align with increasing global case reports suggesting a trend of previously healthy individuals developing POTS after mRNA COVID-19 vaccinations. One report details a 42-year-old male with no previous POTS symptoms who developed the condition following his first mRNA COVID-19 vaccine dose.
The findings may be associated with the operation of mRNA vaccines. These vaccines utilize a snippet of the virus’s genetic code to create a protein in our cells, prompting the immune system to generate antibodies.
“The formation of antibodies triggers an autoimmune response that stimulates POTS disease,” the report’s authors wrote.
A detailed study in Nature Cardiovascular Research, published in December 2022, also identified a potential correlation between POTS and COVID-19 vaccination but highlighted a stronger link between POTS and the residual effects of a SARS-CoV-2 infection.
Using a dataset of 284,592 vaccinated individuals, 93 percent of whom received the mRNA vaccine, the study found a 33 percent increase in the likelihood of developing POTS. More than half of the 4,526 total POTS diagnoses occurred after vaccination.
“POTS-related diagnoses appear to be acquired with increased frequency after, compared to before, COVID-19 vaccination, particularly when compared to more commonly diagnosed conditions, but at a rate that is approximately five times lower than after SARS-CoV-2 infection,” the authors concluded.
The authors cautioned against using the study results to avoid vaccination.
“These study results are not intended to discourage use of the COVID-19 vaccine, especially given the relatively higher risk of developing POTS after SARS-CoV-2 infection,” they wrote.
The Health Care Hurdles Facing POTS Patients
Amid a health care system strained by the aftermath of a global pandemic, POTS patients confront issues of time and resources.
“We’re facing a backlog of over two years just to get patients into our treatment center,” Dr. Chung said.
Despite its global impact on millions, POTS remains largely unknown to many health care professionals, often resulting in a lengthy and challenging path to an accurate diagnosis. A 2013 survey by Dysautonomia International highlighted this struggle for more than 700 POTS patients.
On average, patients face a six-year delay before receiving a correct diagnosis. Only 25 percent are diagnosed within the first year of symptom onset, and many travel more than 100 miles for POTS-related medical care. Further complicating matters, 59 percent of patients are initially dismissed by doctors who believe that their severe symptoms are purely psychological.
Dr. Chung highlights many other hurdles that POTS patients face—a lack of awareness, elusive biomarkers, limited treatment options, and debilitating disease severity.
Yet he underscores a critical roadblock.
“While my view may be biased, I believe the dearth of research funding presents one of the most formidable challenges for advancing POTS care,” Dr. Chung told The Epoch Times.
Multifaceted Treatment Approach for POTS Patients
One of the complexities in treating POTS arises from the stark variations in individual symptoms, necessitating a personalized treatment strategy. At the Johns Hopkins POTS Treatment Center, the process begins with a patient-centric focus, devising strategies that range from subtle lifestyle adjustments to the use of medications.
A vital cornerstone of this strategy involves enhancing fluid intake to bolster blood volume and adjusting daily activities, such as altering how patients move from sitting to standing. Physical therapy exercises, tailored to suit each patient’s tolerance levels, are also integral to the therapeutic regimen.
The role of medication is twofold, targeting both POTS symptoms and any underlying conditions. This could encompass the use of beta-blockers or other heart rate-reducing drugs. For some, medications that amplify the body’s ability to absorb salt and fluid or those promoting blood vessel constriction to improve blood flow to the heart and brain may be recommended.
The prescription of dietary modifications, such as increased salt intake and hydration, form another line of attack, providing symptomatic relief. A small Vanderbilt University study corroborates this approach, demonstrating symptom improvement in POTS patients on a high-salt diet, although it fell short of complete symptom eradication.
Compression stockings have shown promise in aiding POTS management by helping to improve blood flow and alleviate symptoms. Ms. Eaton championed this intervention.
“Compression leggings really help in managing my day-to-day symptoms,” she said.
The final crucial element of the approach involves counseling, providing patients and their families with practical strategies to manage life with POTS.
Addressing POTS With Holistic Approaches
While conventional medicine typically focuses on managing POTS symptoms, there’s a shift toward targeting the root causes.
POTS Care in Texas pioneers this approach by integrating biofeedback, specialized supplements, and low-inflammatory diets into its treatment. Biofeedback, a noninvasive method, enables patients to control bodily functions such as heart rate. The facility provides personalized supplement regimens to meet individual nutritional needs and recommends a low-inflammatory diet to minimize symptom triggers.
“Our efforts go towards locating and treating the underlying cause of POTS and its numerous comorbid conditions,” the clinic’s website reads.
The goal extends beyond symptom relief—it aims for lasting, sustainable health improvement.
Board-certified cardiologist Dr. Jack Wolfson, lauded for his success in treating POTS patients through natural methods, runs the Natural Heart Doctor clinic. Known for his affinity toward holistic therapies, Wolfson echoes the ethos of POTS Care, setting a firm stance on curative over symptomatic treatment.
“POTS is an inflammatory condition at its core,” Dr. Wolfson told The Epoch Times. “Our approach is about identifying and treating the cause. For some patients, it’s mold toxicity. For others, it’s a high burden of other toxins. Still, for others, it’s an imbalance in the nervous system. We’ve seen remarkable progress in our patients by directly addressing these factors.”
The move toward alternative treatments and a deeper comprehension of POTS signals a fresh chapter in managing this intricate syndrome. Despite the ongoing challenge of fully understanding POTS, integrating alternative therapies with traditional methods offers renewed hope for many patients.
Reposted from: https://www.theepochtimes.com/health/the-rise-of-pots-in-the-covid-19-and-vaccine-era-5383977
Read more articles related to vaccine: Vaccine series.






.png)

Comments
Post a Comment