2 Types of Vaccinated or Long-COVID Patients Have a Higher Risk of Blood Clots
People grappling with long COVID and vaccine injury have one potential problem to worry about: blood clots. Some are more likely to find themselves caught up in this conundrum than others, and the reason may be beyond their control.
Tiny blood clots, often called microclots, can wreak havoc on the body. Forming in small blood vessels, they obstruct the flow of vital nutrients and oxygen, leaving a trail of breathlessness, brain fog, and exhaustion in their wake.
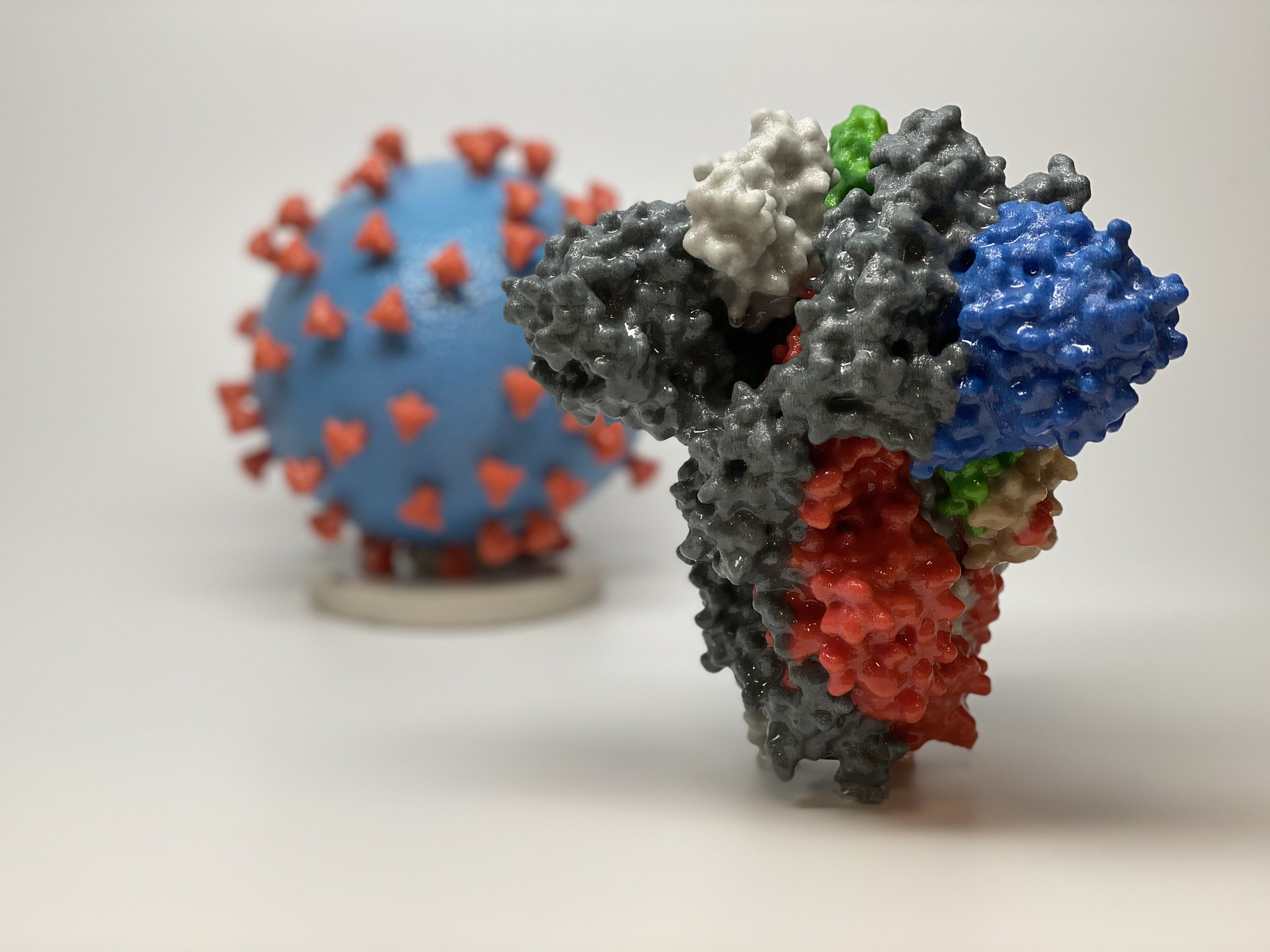 |
| This image shows a 3D print of a spike protein of SARS-CoV-2—the virus that causes COVID-19—in front of a 3D print of a SARS-CoV-2 virus particle. (Courtesy of NIAID/RML) |
Researchers may already have most of the answers as to why and how microclotting occurs in long-COVID and vaccine-injured patients. More recent studies have also identified that individuals with specific conditions or genes may be at a higher risk of injury.
Who Is Predisposed to More Severe Outcomes?
People with underlying comorbidities, such as being overweight, diabetes, and cardiovascular disease, experience higher levels of inflammation, increasing their susceptibility to microclotting caused by COVID-19 infection or vaccination.
This is because inflammation activates platelets, tiny blood cells that help the body form clots. Even before the onset of COVID-19, research has associated these common comorbidities with clotting complications.
COVID-19 infection and its vaccines may induce microclotting through the spike proteins they produce. Spike proteins are surface proteins found in the COVID-19 virus. The COVID-19 mRNA vaccines also prompt the body’s cells to generate spike proteins.
Spike proteins can trigger microclotting through several pathways:
- Induce blood clotting by infecting and damaging the endothelial cells that line the inner blood vessels.
- Activate blood clotting spontaneously in the absence of thrombin and platelets.
- Change the structure of proteins involved in clotting, resulting in large amyloid structures impervious to breakdown.
“That said, we are also finding a huge number of individuals who had no previous comorbidities, who were perfectly healthy [who have trouble recovering from long COVID],” Etheresia Pretorius, a distinguished research professor specializing in microclotting at Stellenbosch University, told The Epoch Times. This includes athletes, prompting Ms. Pretorius to propose that genetic factors may also be involved in these instances.
Genetics: A Major Risk Factor for Microclotting
1. MTHFR Mutations
MTHFR is an abbreviation for methylenetetrahydrofolate reductase, a protein involved in the body’s folate (vitamin B9) processing.
Mutations to the MTHFR gene produce a dysfunctional MTHFR protein and can result in folate deficiency and elevated homocysteine (a type of amino acid) levels, both associated with a higher risk of blood clotting.
Doctors can test for MTHFR mutations using a blood test, and several studies have shown that long-COVID patients tend to carry the MTHFR mutation. This mutation is also quite common among patients with COVID-19 vaccine injuries, so patients with this gene may fare worse after COVID-19 infection or vaccination.
Individuals with two copies of the mutated MTHFR gene may have an increased susceptibility to microclotting, according to research led by Ms. Pretorius and Professor Douglas Kell, a system biologist from the University of Liverpool (pdf).
2. Mutation of a Protein Involved in Blood Clotting
Mutations in the plasminogen activator inhibitor-1 (PAI-1), a protein involved in normal blood clotting, are a risk factor for microclotting in long COVID and vaccine injury, board-certified internist Dr. Jordan Vaughn told The Epoch Times. Studies have demonstrated that in acute COVID-19 cases, PAI-1 levels become elevated.
Dr. Vaughn has detected these mutations through patient screenings. Of his 210 long-COVID patients, 189 were found to carry the PAI-1 gene mutations, Dr. Vaughn said during his presentation at the April Frontline COVID-19 Critical Care (FLCCC) Alliance conference.
These mutations increase PAI-1 protein production, leading to higher levels of PAI-1 in the bloodstream, thereby increasing the risk of blood clots.
The genetic polymorphism can be identified by analyzing a blood sample.
Caucasians and East Asians are at the highest risk of carrying these genes, Dr. Vaughn said.
Elevated PAI-1 levels are also commonly observed in older individuals and can be influenced by age-related health conditions such as obesity, insulin resistance, hypertension, psychological stress, and immunological diseases.
Dr. Vaughn added that people with a family history of strokes and arteriosclerosis are more likely to carry PAI-1 mutations. He also suggested that those with PAI-1 gene polymorphisms and individuals with known family history might benefit from taking anti-platelet and anticoagulant medications preventively.
Detecting Microclots
There is no approved quantitative test to determine if a person has microclotting. Since many inflammatory proteins remain trapped in the clots rather than dissolved inside the plasma, tests for clots may come back negative even though patients have microclots present.
However, Ms. Pretorius and Mr. Kell’s team has developed a laboratory technique that allows researchers to detect microclots using fluorescent microscopes.
The advanced equipment used, however, would mean that the test cannot be made commercially available.
“Unfortunately, it’s just research laboratories [that can do this test] because fluorescent microscopes are not necessarily present in a general pathology lab,” Ms. Pretorius told The Epoch Times over a video call.
A few doctors have even acquired their own fluorescent microscopes and started doing the tests themselves.
The microscope testing, however, only detects microclots; it provides no answers about the severity of the condition. Researchers can’t know the average size of the microclots nor the number of clots in the sample.
But a test that is more clinically robust and accessible may be coming soon.
Ms. Pretorius and Mr. Kell’s team recently developed a new flow cytometry testing method. The preprint on their technique was published in March.
Although general pathology laboratories may not have a fluorescent microscope, most have a flow cytometer. A flow cytometer is usually used to detect cancer cells. The blood or tissue sample is first tagged for cancer markers, then the flow cytometer examines the cells one by one for the same markers and provides a reading on the number and size of the cancer cells detected.
If the flow cytometry test proves to be successful, it may also work for detecting microclots.
In their report, Ms. Pretorius and Mr. Kell’s team dyed a plasma sample with thioflavin, which binds to amyloid proteins, including microclots.
The sample was then spun through the flow cytometer, and its readings found that compared to healthy people, samples taken from long-COVID patients had higher readings of thioflavin, suggesting more microclots in the blood for long-COVID patients.
Research on Microclotting’s Role in Chronic Diseases Is Needed
Addressing blood clotting could have a pivotal role in preventing various chronic diseases, Dr. Vaughn said, leading him to anticipate a significant emphasis on microclotting in health care in the future.
Ms. Pretorius said she hoped further investigations would shed light on the persistent nature of blood clots in these conditions.
“I think there has been a huge neglect by researchers and clinicians over the years to closely examine conditions like diabetes and rheumatoid arthritis and the role of abnormal clotting in these diseases,” she added. “Perhaps it’s now time to focus on clotting pathologies in these diseases and find answers to many of the persistent symptoms in these individuals.”
Read more articles related to spike protein > Spike Protein series
Reposted from: https://www.theepochtimes.com/health/2-types-of-vaccinated-or-long-covid-patients-have-a-higher-risk-of-blood-clots_5379346.html






.png)

Comments
Post a Comment