Myocarditis: Symptoms, Causes, Diagnosis and Treatments
Myocarditis is inflammation of the myocardium, the muscular layer of the heart. This inflammation can weaken the heart and make it less able to pump blood effectively.
Severe myocarditis can weaken the heart to the point that the body doesn’t get enough oxygen. Sluggish muscle contraction and pooling of blood in the heart may result in clots that could travel to the brain, causing a stroke, or to the coronary blood vessels of the heart, causing a heart attack.
The global annual prevalence of myocarditis is estimated to be approximately 17 per 100,000 individuals. The clinical presentation of this disease varies, as does individual outcome. According to a paper published in Circulation: Heart Failure, most cases resolve spontaneously; however, some patients experience severe heart damage that could lead to death.
What Are the Common Types of Myocarditis?
Myocarditis can be categorized based on the cause, phase, predominant symptoms, and cellular pathology. The diagnostic criteria are continuously changing as researchers gain more insight that evolves our understanding of the disease.
Let’s look at some essential terms associated with different types of myocarditis.
Acute Versus Chronic
- Acute: In this classification, symptoms began within the past month.
- Chronic: Symptoms of myocarditis have been present for longer than one month.
There are also classifications based on how the tissue looks under a microscope (histological presentation):
- Lymphocytic: This is the most frequent form seen in histological review and includes autoimmune and viral forms.
- Neutrophilic: This type of myocarditis includes fungal, bacterial, and early stages of viral myocarditis. With this form, white blood cells called neutrophils move into the myocardium of the heart and infiltrate an area with acute inflammation.
- Granulomatous: Granulomas are small clusters of immune cells that form as a reaction to infections or other irritants. This type of myocarditis includes giant-cell myocarditis. Giant-cell myocarditis is defined by extensive cell infiltrates and the presence of giant cells that have moved into the myocardium. Sarcoidosis (collections of inflammatory cells that form lumps) is a frequent cause of granulomatous myocarditis.
- Eosinophilic: According to the Circulation: Heart Failure paper, eosinophilic myocarditis is the most common type of hypersensitivity myocarditis, which occurs when the myocardial damage is caused by a reaction to a drug. Eosinophils are associated with allergic response and hypersensitivity myocarditis is also referred to as allergic myocarditis.
What Are the Symptoms and Early Signs of Myocarditis?
Symptoms may develop slowly or happen very quickly and may include:
- Fatigue
- Chest pain
- Rapid or irregular heartbeat
- Shortness of breath
- Flu-like symptoms such as body aches, fever, or sore throat
- Swelling of the legs and feet
Symptoms of myocarditis in children include:
- Difficulty breathing
- Chest pain
- Fever
- Fainting
- Rapid or irregular heartbeat
If you or your child experience symptoms of myocarditis, it is important to seek medical attention right away, particularly if the symptoms include unexplained chest pain, shortness of breath, or rapid heartbeats.
What Causes Myocarditis?
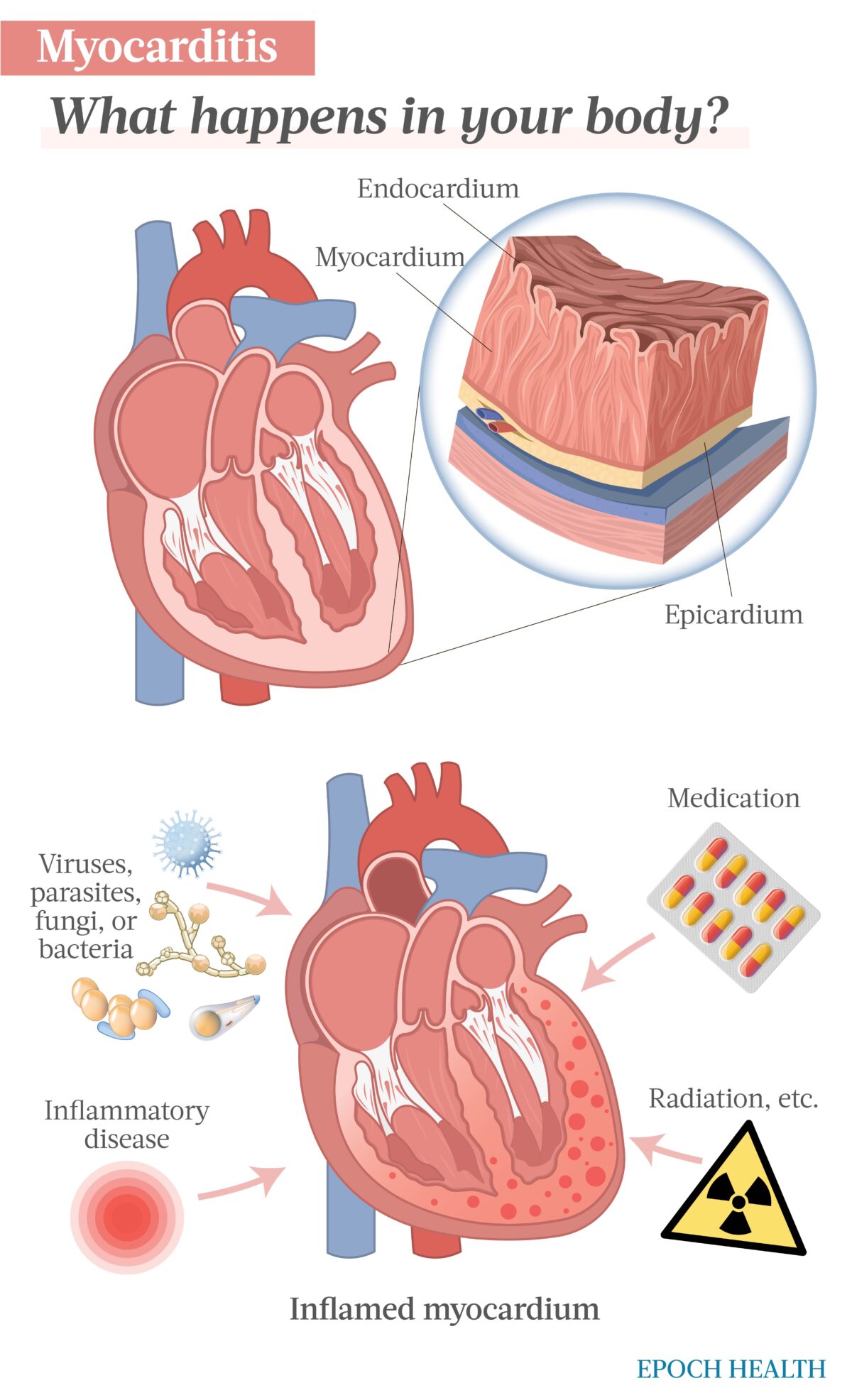
Three distinct layers make up the heart wall. The innermost layer is the endocardium, the middle layer is the myocardium, and the outermost layer is the epicardium. The epicardium is part of the pericardium, a structure that surrounds and protects the heart.
The myocardium is the thickest and strongest layer of the wall of the heart.
Myocarditis refers to inflammation in the myocardium that is not a result of low oxygen supply or a reaction to organ transplantation. It occurs as a result of infection, immune system activation, or exposure to toxic substances.
Myocarditis can be caused by viral, parasitic, bacterial, or fungi infections, diseases that cause inflammation, certain medications, and exposure to certain chemicals.
- Viruses: Viral infection is the most prevalent cause of myocarditis. Viruses that have been linked to myocarditis include COVID-19, influenza viruses, adenovirus (causes the common cold), hepatitis B and C, coxsackie viruses, echoviruses (cause gastrointestinal sickness), rubella virus, herpes viruses, parvovirus (associated with fifth disease), and human immunodeficiency virus (HIV).
- Parasites: Certain parasites can cause myocarditis. Toxoplasma is a parasite that can get into the body by consumption of undercooked meat or through contact with cat feces. This parasite is a potential cause of myocarditis. Trypanosoma cruzi is a parasite found in the feces of the triatomine bug. Its feces contaminates a nearby bite by the same bug on the skin. Infection with Trypanosoma cruzi is a potential cause of myocarditis. Plasmodium falciparum—the protozoan that causes malaria—is another cause of myocarditis.
- Bacteria: Several types of bacteria can cause myocarditis. These include streptococcus, staphylococcus, chlamydia, Borrelia burgdorferi (known to cause Lyme disease), and Corynebacterium diphtheriae (known to cause diphtheria).
- Fungi: A fungus may cause myocarditis, though this is rare. These fungi include Aspergillus (a mold), Candida (a yeast), and Histoplasma (found in bird waste).
- Inflammatory disease: Rheumatoid arthritis, lupus, Takayasu’s arteritis (a rare type of vasculitis), Wegener’s granulomatosis (a rare blood vessel disease), and sarcoidosis are diseases that contribute to body-wide inflammation and may cause myocarditis.
- Medications: Some cancer treatment medications, such as immune checkpoint inhibitor drugs, can cause myocarditis. Some anti-seizure medications and several antibiotics including penicillin may cause myocarditis. In addition, benzodiazepines and anti-psychotic medicines, like clozapine, can cause myocarditis.
- Other: Exposure to radiation, carbon monoxide, heavy metals, certain snake venoms, and cocaine can all cause myocarditis. Furthermore, COVID-19 mRNA vaccination can cause myocarditis.
Who Is More Likely to Get Myocarditis?
You’re more likely to get myocarditis if:
- Your body doesn’t handle inflammation well. It means genetically, you may be more susceptible to myocarditis.
- You drink a lot of alcohol.
- You are undergoing dialysis treatments.
- You have an implanted heart device.
- You are being treated for cancer.
- You have an inflammatory disease such as lupus, rheumatoid arthritis, or sarcoidosis.
What Are the Tests to Detect Myocarditis?
If you are exhibiting symptoms of myocarditis, it is important to be evaluated by a doctor. Early diagnosis is important for protecting your heart from further damage. Evaluation begins with your doctor giving you a thorough physical examination, including listening carefully to your heart.
Your doctor may further evaluate you with the following tests depending on your history and physical exam:
- Bloodwork: A cardiac enzyme test can evaluate whether heart muscle is being damaged. Tests for infections that can cause myocarditis may be ordered.
- Electrocardiogram (ECG, EKG): An EKG will reveal if your heart is not beating correctly (there is an arrhythmia).
- Cardiac magnetic resonance imaging (MRI): This test gives detailed images of the heart and can reveal inflammation in the heart’s muscle tissue.
- Positron emission tomography (PET) scan: This test can reveal the shape and size of the heart as well as some of its level of function.
- Echocardiogram: This test allows the doctor to see how well blood is flowing through the heart.
- Heart muscle biopsy: In this test, a tiny sample of heart muscle tissue is taken and sent to the lab for analysis.
- Chest X-ray: This evaluates whether there is fluid around the heart that could be indicative of heart failure.
What Are the Complications of Myocarditis?
Frequently, myocarditis subsides without ongoing complications; however, in some individuals, it may cause life-threatening, extensive complications.
- Stroke or heart attack: Severe myocarditis may damage the heart muscle to the point where the heart cannot pump blood effectively. Pooling blood in the heart may result in clots that could travel to the brain, causing a stroke, or travel to the coronary blood vessels of the heart, causing a heart attack.
- Heart failure: Damage to the heart muscle may be severe enough that the heart cannot pump blood effectively. In some cases, this heart failure may result in the need for a ventricular assist device to pump blood efficiently. In more severe cases, a heart transplant may be needed.
- Rapid or irregular heart rhythms (arrhythmias): Damage to the heart muscle can cause irregularities in the heartbeat. Some arrhythmias can lead to further strain on the heart, blood clots, or inability to pump.
- Cardiac arrest: Certain arrhythmias can result in the heart not being able to beat at all (sudden cardiac arrest). This is deadly unless treated immediately.
What Are the Treatments for Myocarditis?
Treatment depends on the severity of myocarditis. Rest is crucial for anyone with this condition. In addition, your doctor may prescribe medication or therapy.
Medications and Therapies
- Medications to treat ongoing conditions: If you have an inflammatory disease, your doctor may prescribe a medication to help treat the inflammatory disease. For instance, rituximab is a monoclonal antibody that targets CD20 B lymphocytes and is used to treat autoimmune disorders, such as rheumatoid arthritis and lupus. Researchers believe rituximab may be useful for treating myocarditis patients who do not respond to steroids, according to a paper in the journal Circulation Research.
- Immunosuppressive therapy: Immunosuppressants help mitigate the damage of the immune system on healthy cells and tissues. According to the Circulation Research paper, studies suggest immunosuppressive therapy with azathioprine and prednisone helps improve cardiac function in myocarditis patients who do not have evidence of a viral component in their myocarditis (based on tissue biopsy). Some treatment regimens include a steroid-based protocol in combination with cyclosporine.
- Medications that reduce the risk of clots: If blood is pooling in your heart due to inadequate pumping, your doctor may prescribe a medication that helps keep your blood from clotting. Anticoagulants, such as warfarin and heparin, slow down the process of making clots. Antiplatelet drugs, such as aspirin, help keep platelets from clumping together to form a clot.
- Heart medications: Some medications reduce the strain on the heart by removing extra fluid from the body. If your heart is weak, your doctor may prescribe a diuretic, angiotensin-converting enzyme (ACE) inhibitor, or beta blocker. Diuretics include furosemide, bumetanide, and several others. ACE inhibitors help relax veins and arteries to lower blood pressure. Some examples of ACE inhibitors include benazepril, enalapril, and lisinopril.
- Interferon therapy: Data suggest that immunomodulatory interferon-beta injections can help accelerate virus clearance or reduce viral load in patients experiencing enterovirus and adenovirus-induced myocarditis.
- Intravenous (IV) immunoglobulin: Intravenous immunoglobulin (a pool of IgG, IgA, and IgM antibodies) has antiviral and anti-inflammatory effects and may help regulate cytokines that are contributing to myocyte death. One meta-analysis revealed this type of antibody therapy resulted in decreased in-hospital death rates and helped left ventricular function recovery in acute myocarditis patients.
Procedures and Devices
If you are experiencing severe myocarditis, you may need one of the following treatments:
- Left ventricular assist device (LVAD): This device aids your heart in pumping blood out of the left ventricle—the left lower chamber of the heart—to the rest of the body.
- Pacemaker: If the heart is beating irregularly due to damage from myocarditis, it may become necessary to have an artificial pacemaker inserted to regulate heart rhythm.
- Extracorporeal membrane oxygenation (ECMO): During ECMO, blood circulates out of your body, passes through the ECMO machine, and then returns to your body. When a portion of blood passes through the ECMO machine, carbon dioxide is removed and replaced with oxygen. In cases of severe heart failure, this machine may be necessary to keep the patient alive.
- Heart transplant: Sometimes the heart is damaged beyond repair and a heart transplant becomes necessary.
How Does Mindset Affect Myocarditis?
Ongoing stress can contribute to inflammation. It’s important to find stress-reducing activities to lower your stress levels and help lower inflammation. Various methods to help reduce stress can be incorporated into your daily life, such as:
- Journaling.
- Being outside in nature for 20 minutes.
- Stretching your muscles.
- Taking a brisk walk.
- Having a cup of warm tea.
- Reading or watching something funny.
- Playing soothing music.
- Thinking about three things for which you are thankful.
- Writing a list of goals.
- Taking deep, relaxing breaths.
What Are the Natural Remedies for Myocarditis?
Several nutraceuticals show promising results in the treatment of myocarditis:
- Polyphenols: This large group of phytochemicals can be found in a range of fruits, vegetables, and grains. Quercetin is a polyphenol pigment that is found in many fruits and vegetables. It is a powerful antioxidant present in onions, apples, blueberries, kale, broccoli, and other foods. Chrysin is a polyphenol found in many plants such as passionflowers and mushrooms, as well as honey.
- Alkaloids: This group of phytochemicals may help prevent oxidative stress and inflammation. It includes berberine, found in traditional herbal medicines (Hydrastis canadensis, Berberis, and Coptis). It also includes colchicine, which is derived from autumn crocus.
- Terpenoids: This class of nutriceuticals includes Ginkgo biloba and Astragaloside IV, found in Astragalus membranaceus. Astragalus membranaceus is a key medicinal herb used in traditional Chinese medicine. It is known to have antioxidant and anti-inflammatory effects. One review noted that 28 randomized controlled trials on the effect of the herb on viral myocarditis revealed that Astragalus membranaceus “exerted cardioprotective function in [viral myocarditis-infected] animals and patients largely through antivirus and antivirus receptors, anti-inflammatory, antioxidation, anti-apoptotic, anti-fibrosis, and reducing cardiac calcium load.”
Please consult with a health care professional before supplementing with herbs.
How Can I Prevent Myocarditis?
While there is nothing you can do that will be 100 percent effective in preventing myocarditis, you can take certain steps to decrease your risk of infection, which helps decrease your overall risk of myocarditis.
- Stay away from people who are sick.
- Avoid risky behaviors that could expose you to HIV, hepatitis B, and chlamydia.
- Avoid being exposed to radiation, heavy metals, and carbon monoxide.
- Ensure your meat is properly cooked.
- Avoid exposure to animal feces.
Medical reviewed by Beverly Timerding, M.D..
Reposted from: https://www.theepochtimes.com/health/the-essential-guide-to-myocarditis-symptoms-causes-treatments-and-other-remedies_5168016.html






.png)

Comments
Post a Comment