Meta-Analyses Confirm Vitamin D Defends Against COVID (2022)
In all cases, the data consistently show that low vitamin D levels raises your risk of COVID while higher baseline levels and/or supplementation lowers all risks by 1.5 to three times.
Therapeutic Role of Vitamin D in COVID
In the first of these four meta-analyses, “Prognostic and Therapeutic Role of Vitamin D in COVID-19: Systematic Review and Meta-Analysis,” published December 11, 2021, the researchers sought to determine “the association between vitamin D deficiency/insufficiency and susceptibility to COVID-19, its severity, mortality and role of vitamin D in its treatment.”
A total of 72 observational studies, covering 1,976,099 patients, met the criteria for inclusion. Compared to those with sufficient vitamin D, the odds of developing COVID-19 among those with deficient or insufficient vitamin D levels were 1.46 times higher.
Their risk of severe disease was also 1.9 times higher, and their risk of death 2.07 times higher. One potential drawback was that all studies ranked “high” for risk of bias. The studies also differed in their definitions of severe illness and vitamin D deficiency/insufficiency, making absolute comparisons difficult. That said, the authors concluded:4
“Multiple observational studies involving nearly two million adults suggest vitamin D deficiency/insufficiency increases susceptibility to COVID-19 and severe COVID-19, although with a high risk of bias and heterogeneity. Association with mortality was less robust.”Vitamin D Status and Clinical Outcomes
In the second study, “Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes,”5 published December 22, 2021, the researchers assessed “whether vitamin D status is associated with the COVID-19 severity, defined as ARDS requiring admission to intensive care unit (ICU) or mortality (primary endpoints) and with the susceptibility to SARS-CoV-2 and COVID-19-related hospitalization (secondary endpoints).”
Here, they included 54 observational studies (1,403,715 patients) that measured the association between vitamin D status and risk of COVID infection, hospitalization, ICU admission and death during hospitalization. The measures for vitamin D status were as follows:
- Insufficiency — less than 75 nmol/L (30 ng/mL)
- Deficiency — less than 50 nmol/L (20 ng/mL)
- Severe deficiency — less than 25 nmol/L (10 ng/mL)
Seventeen studies reported the association between vitamin D status and SARS-CoV-2 infection; nine reported the association with COVID-19 related hospitalization, 27 reported COVID-19-related ICU admission, and 35 reported COVID-19 related mortality. In summary, the odds of ICU admission based on vitamin D status were as follows:
- Severe deficiency — 2.63 times higher
- Deficiency — 2.16 times higher
- Insufficiency — 2.83 times higher
Those with severe deficiency were also 1.68 times more likely to test positive; those with deficiency were 1.83 times more likely to test positive; and those with insufficiency were 1.49 times more likely to test positive. In conclusion, the authors stated:6
“Patients with low vitamin D levels present an increased risk of ARDS requiring admission to intensive care unit (ICU) or mortality due to SARS-CoV-2 infection and a higher susceptibility to SARS-CoV-2 infection and related hospitalization.”The Effect of Vitamin D Supplementation
The third study, “The Effect of Vitamin D Supplementation on Mortality and Intensive Care Unit Admission of COVID-19 Patients. A Systematic Review, Meta-Analysis and Meta-Regression,”7 was published in May 2022.
The effect of vitamin D supplementation was found to be quite significant — 12.19% of patients who received vitamin D required ICU admission, compared to 26.27% of those who did not get vitamin D.Six studies, involving 860 patients, had data on ICU admission. Of those 860 patients, 369 received vitamin D supplementation and 491 did not, and the effect of vitamin D supplementation was found to be quite significant — 12.19% of patients who received vitamin D required ICU admission, compared to 26.27% of those who did not get vitamin D.
The data in all six studies strongly favored vitamin D. The ideal dose, however, remains uncertain, as no linear relationship between dose and odds ratio of ICU admission was observed.
Vitamin D and SARS-CoV-2 Infection, Severity and Mortality
The fourth and most recent study, “Vitamin D and SARS-CoV-2 Infection, Severity and Mortality: A Systematic Review and Meta-Analysis,”8 was published July 6, 2022, in PLOS ONE.
Here, they looked at COVID-19 in relation both to baseline vitamin D status and supplementation. Thirty-eight studies — including two randomized controlled trials — were included that had risk estimates for at least one endpoint (risk of infection, severity and/or mortality). In all, data on vitamin D status was available for 205,565 patients and 2,022 who were given vitamin D supplementation. According to the authors:9
“Random effects models showed that supplementation was associated with a significant lower risk of both COVID-19 severe disease (SRR 0.38, 95% CI 0.20-0.72, 6 studies) and mortality (SRR 0.35, 95% CI 0.17-0.70, 8 studies).There were no statistically significant dose differences between studies: summary estimates with regular doses remain statistically significant, suggesting that higher doses are not necessary. For patients on vitamin D supplementation, a greater reduction in mortality risk emerged in older individuals and at higher latitudes.
Regarding the quality of studies, assessed using the New Castle-Ottawa quality scale, the analysis revealed in most cases no statistically significant differences between low, medium or high quality studies.
We found significant associations of vitamin D supplementation with COVID-19, encompassing risks of disease worsening and mortality, especially in seasons characterized by 25OHD deficiency and with not severe patients.”
Why Randomized Controlled Trials Are Not Required
As noted by in a Twitter thread by Karl Pfleger, Ph.D., the data clearly show vitamin D is strongly correlated with all COVID-19 risks, and we do not actually need randomized controlled trials to draw this conclusion:10
“Most underlying studies are observational, but at the very least knowledge of whether someone supplements D or of their D status is strongly predictive of their COVID risks/outcomes. As I've noted previously, RCTs are not required for this conclusion to be sound & unquestionable. This establishes a risk factor & most other well known COVID risks factors are also based entirely on observational data.The data showing age, above-normal-weight, & comorbidities are significant risk factors is also based entirely on correlation. No RCTs establish these as risk factors but no one questions that they are. VDD [vitamin D deficiency] should be thought of as another comorbidity, just like diabetes.”
Indeed, at this point, the importance of vitamin D in the fight against COVID ought to be common knowledge everywhere, especially in health care circles. Yet the surgeon general of Florida, Joseph Ladapo, is the only public health official who is actually recommending vitamin D optimization for COVID.11
This is crazy, as the effects of vitamin D were evident very early on in the pandemic. I launched an information campaign about vitamin D back in June 2020, which included the release of a downloadable scientific report that detailed the science behind vitamin D. This report, as well as a two-minute COVID risk quiz is available on StopCovidCold.com.
In December 2020, more than 100 doctors, scientists, Ph.D.’s and leading authorities from 33 countries also signed an open letter12 to the governments and health officials of the world, calling for the use of vitamin D against COVID. Since then, the list of signatories has grown to 220.
The letter recommended taking enough vitamin D to achieve a blood level of at least 30 ng/mL (75 nmol/L), urged testing of all hospitalized COVID-19 patients and adding vitamin D to the treatment protocol for any patient whose level was below 30 ng/mL.
Not only did health agencies roundly ignore this sound advice, but they also publicly tried to discredit the notion that vitamin D could have any benefit at all, and attacked anyone sharing the good news about vitamin D.
As just one example, in the summer of 2020, the Center for Science in the Public Interest (CSPI), a self-proclaimed consumer advocacy group bankrolled by the Rockefeller Foundation, among others, launched a campaign against Mercola.com. The CSPI falsely accused me of “profiteering from the pandemic” by selling nutritional supplements, including vitamin D, while sharing scientific truth about its benefits.
The campaign culminated in a warning letter from the U.S. Food and Drug Administration, in which they warned me to stop talking about vitamin D. I reviewed this censorship attempt in “Why Is Info on COVID and Vitamin D Deficiency Suppressed?”
The fact of the matter is, data show vitamin D supplementation lowers your risk of a positive test, speeds viral clearance, slows the spread of infection, and lowers your risk of severe infection, hospitalization and death, as summarized in “Vitamin D Deficiency and COVID-19 Severity” and many other articles.
Mechanisms Behind Vitamin D
At the end of October 2020, I published my own vitamin D review13 in the peer-reviewed journal Nutrients, co-written with William Grant, Ph.D., and Dr. Carol Wagner, both of whom are part of the GrassrootsHealth expert vitamin D panel. You can read the paper for free on the journal's website.
As noted in that paper, dark skin color, increased age, preexisting chronic conditions and vitamin D deficiency are all features of severe COVID disease and, of these, vitamin D deficiency is the only factor that is readily and easily modifiable.
You may be able to reverse chronic disease, but that typically takes time. Optimizing your vitamin D, on the other hand, can be achieved in just a few weeks, thereby significantly lowering your risk of severe COVID-19.
In our paper, we review several of the mechanisms by which vitamin D can reduce your risk of COVID-19 and other respiratory infections, including but not limited to the following:14
- Reducing the survival and replication of viruses15 and inflammatory cytokine production
- Maintaining endothelial integrity — Endothelial dysfunction contributes to vascular inflammation and impaired blood clotting, two hallmarks of severe COVID-19
- Increasing angiotensin-converting enzyme 2 (ACE2) concentrations, which prevents the virus from entering cells via the ACE2 receptor — ACE2 is downregulated by SARS-CoV-2 infection, and by increasing ACE2, you also avoid excessive accumulation of angiotensin II, a peptide hormone known to increase the severity of COVID-19
Vitamin D is also an important component of COVID-19 prevention and treatment for the fact that it:
- Boosts your overall immune function by modulating your innate and adaptive immune responses and reduces respiratory distress16 and improves overall lung function
- Regulates inflammatory cytokine production, which is one of the lethal hallmarks of COVID-19
- Helps produce surfactants in your lungs that aid in fluid clearance17 and lowers your risk of comorbidities, including obesity,18 Type 2 diabetes,19 high blood pressure20 and heart disease21
Data from 14 observational studies — summarized in Table 1 of our paper22 — suggest that vitamin D blood levels are inversely correlated with the incidence and/or severity of COVID-19 and, importantly, that the evidence currently available generally satisfies Hill's criteria for causality in a biological system.23
Why Sun Exposure Is the Best Way to Optimize Vitamin D
The ideal way to optimize your vitamin D level is by exposing large portions of bare skin to the sun. I take an hour-long walk during solar noon every day, wearing just shorts and a baseball cap, and have not needed oral vitamin D supplementation for over 13 years.
This is not some theoretical obsession I have. I am now beyond convinced that swallowing vitamin D is exponentially inferior to getting it from the sun. I would encourage you to do everything in your power to get it from the sun. And, when you get it from the sun, you should not be swallowing it.
It is important to regularly check your vitamin D levels to see how you are doing with your program. Ideally, your level should be between 60 ng/mL and 80 ng/mL. Last week my vitamin D level was 100, the first time ever in my life I was in the triple digits, and all with no oral supplementation for over a dozen years. Remember, vitamin D is a biomarker for all the good things the sun does for you.
I believe this is largely because I was diligent this year to time the middle of my daily walk around solar noon. Since I live in FL, which practices daylight savings time, solar noon, is 1 PM. So I typically start my walk around 12:30 and finish around 70-90 minutes later. Last year I went out 1-2 hours earlier and my levels were only around 70, so you can see the importance of timing.
Sun exposure also provides other biological health benefits over and beyond vitamin D production. If the science of sun exposure interests you, check out Dr. Roger Seheult’s MedCram lecture above. In it, he explains the ins and outs of how sunlight impacts your health. One really important health benefit you can only get from sunlight and not oral supplementation is mitochondrial melatonin production.
The best review of the sun’s effect on melatonin is the February 2020 paper,24 “Melatonin in Mitochondria: Mitigating Clear and Present Dangers,” published in the Physiology journal. It’s written by the best researcher in melatonin, Russel Reiter, Ph.D.
Reiter’s key finding is that 95% of the melatonin your body produces is made inside your mitochondria in response to near-infrared (IR) radiation from the sun or other near IR sources. Only 5% of melatonin is produced in your pineal gland.
Melatonin is a master hormone,25 a potent antioxidant26 and antioxidant recycler,27 and a master regulator of inflammation and cell death.28 These functions are part of what makes melatonin such an important anticancer molecule.29
So, to produce melatonin inside your mitochondria actually makes perfect sense, as your mitochondria desperately need protection from the damage caused by oxidative stress produced in the electron transport chain.
In summary, your mitochondria produce ATP, the energy currency of your cells. A byproduct of this ATP production is reactive oxidative species (ROS), which are responsible for oxidative stress. Excessive amounts of ROS will damage your mitochondria, contributing to suboptimal health, inflammation and chronic health conditions such as diabetes, obesity and thrombosis (blood clots).
The good news is your body has a built-in way to counteract these ROS. Inside your mitochondria, you also have an antioxidant system, and the main antioxidant is melatonin.
Melatonin also upregulates your glutathione pathway, which is another potent antioxidant pathway shown to play an important role in COVID. Like vitamin D, glutathione deficiency is associated with COVID severity. In short, your body is well-designed to address oxidative stress, but you need sun exposure in order for that mechanism to work.
One aspect of sun exposure that Seheult did not mention was that it will also increase your testosterone levels naturally. Most people aren’t aware that the highest hormone concentration in men and women is testosterone. Obviously levels are far lower in women, but testosterone is higher than estrogen in women and it is important for optimal biological function — just one more reason why you want to aim for daily sun exposure on as much skin as possible.
Also remember it is not the sun that is the primary cause of sunburn and skin cancer: It is elevated linoleic acid (LA) in the seeds, nuts and seed oils you consume. LA should only be 1% to 2% of daily calories, and it is over 20% in most people. It takes years to lower your LA levels as it stays in your body for about seven years, so start eliminating it from your diet today.
Guidance for Oral Vitamin D Supplementation
If you do opt for oral supplementation, as an absolute last resort, there are additional considerations to take into account. For example, you need 244% more oral vitamin D if you’re not also taking magnesium and vitamin K2,30 so these three should ideally be taken together. You can learn more about this in “Magnesium and K2 Optimize Your Vitamin D Supplementation.”
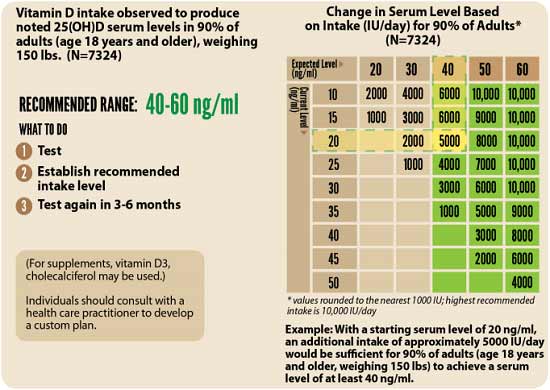
Remember, the most crucial factor when it comes to vitamin D is your blood level, not the dose, as the dose you need is dependent on several individual factors, including your baseline blood level. The level to shoot for is between 60 ng/mL and 80 ng/mL (150 nmol/L to 200 nmol/L); 40 ng/mL should be considered the low-end cutoff.
Before you start oral supplementation, you’ll want to get a baseline measurement. One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit.
Once you know what your blood level is, you can assess the dose needed to maintain or improve your level. The chart below can be helpful. Be sure to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you, and adjust accordingly.
- 1 Google Docs by Karl Pfleger, Ph.D., Meta Analyses List
- 2, 10 Twitter Karl Pfleger August 11, 2022
- 3, 4 J. Clin. Endcrinol. Metab. December 11, 2021; dgab892
- 5, 6 Front. Public Health December 22, 2021; 9: 736665
- 7 Diabetes Metab. Res. Rev. May 2022; 38(4): e3517
- 8, 9 PLOS ONE July 6, 2022; 17(7): e0268396
- 11 Flgov.com December 17, 2021
- 12 VitaminD4all.com December 7, 2020
- 13, 14, 22 Nutrients October 31, 2020;12, 3361; DOI: 10.3390/nu12113361
- 15 Nutrients, 2020;12:988
- 16 Advances in Pharmacological Sciences 2018; 2018: 8494816
- 17 ATS Journals October 5, 2010; 183(10)
- 18 Medicina 2019 Sep; 55(9): 541
- 19 Diabetes.co.uk January 15, 2019
- 20 The Lancet Diabetes & Endocrinology September 1, 2014; 2(9): 682-684
- 21 Current Treatment Options in Cardiovascular Medicine 2012 Aug; 14(4): 414–424
- 23 Nutrients October 31, 2020;12, 3361; DOI: 10.3390/nu12113361, Table 3
- 24 Physiology February 5, 2020 DOI: 10.1152/physiol.00034.2019
- 25 Indian J. Exp Biol. May 1996; 34(5): 391-402
- 26 Frontiers in Pharmacology August 21, 2020 DOI: 10.3389/fphar.2020.01220
- 27 Allergy Research Group, Melatonin, the Antioxidant Recycler
- 28 Cell Death & Disease 2019; 10 article number 317
- 29 Oncotarget June 13, 2017; 8(24): 39896–39921
- 30 GrassrootsHealth Magnesium and Vitamin K2 Combined Important for Vitamin D Levels






.png)

Comments
Post a Comment