Paxlovid vs Molnupiravir (Lagevrio): What are the Differences?
If you are confused about the recommendations made by different professional groups for the COVID-19 pandemic, you've come to the right place.
Are the current treatment options still relevant?
The number of options for the treatment of COVID-19 has increased drastically in recent months, thus making it complicated when it comes to choosing the right combination. In general, there are 3 broad categories of medical interventions:
- Prevention or Prophylaxis e.g. vaccine
- Early out-patient treatment
- Hospital treatment
The medical community themselves are battling over repurposed drugs like ivermectin and hydroxychloroquine on whether they should be used to treat and prevent COVID-19. On one side are experts telling you that more research is needed before the treatment can be fully authorized and confirmed. On the other, are experts telling you that the potential benefits outweigh the risk and a 'wait and do nothing' position is not acceptable. Confused?
How do you deal with different expert groups dishing out conflicting guides? A common issue is that certain groups have pre-defined narrative that they would like to support. Therefore, only studies that support that pre-defined narrative are picked and cited as references. This is what we call as 'cherry-picking'. Cherry picking will naturally lead to a 'biased' and 'manipulated' decision. In order to get the truth out, scientific information needs to be analyzed in a comprehensive, updated and non-biased manner.
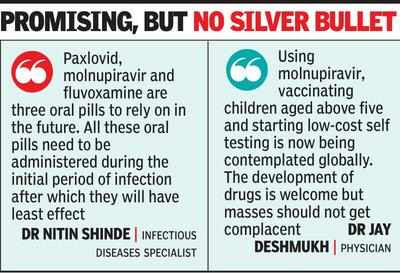
In this article, we will do a roundup and cover 3 popular oral anti-viral treatments i.e. Paxlovid, Molnupiravir and Ivermectin.Contents:
- Paxlovid and COVID-19
- The NIH COVID-19 Treatment Guidelines for High-Risk, Non-hospitalized Patients With Mild to Moderate COVID-19
- Molnupiravir and COVID-19
- Ivermectin and COVID-19
- Ivermectin and FLCCC I-CARE Early Treatment Protocol
- Molnupiravir vs Ivermectin
- Paxlovid vs Ivermectin vs Molnupiravir
Paxlovid and COVID-19
How to Get Paxlovid Without a Medical Doctor
In March 2022, the Biden administration launched the Test to Treat initiative. The initiative’s goal was to allow people to be tested for COVID-19 at
pharmacies or health centers that have an on-site clinic, like CVS
MinuteClinic. If you had a positive test, you’d then receive an antiviral
prescription at the pharmacy before leaving the building.
While
well-intentioned, there were many roadblocks that made the Test to Treat
initiative difficult to roll out. One big barrier was the fact that most
pharmacies don’t have clinics in the same building. In late May 2022,
there were only about 2,500 Test to Treat locations in the entire U.S. This left many Americans still struggling to get
a prescription from their healthcare providers in enough time to benefit
from Paxlovid.
In response to this, the FDA updated Paxlovid’s
EUA in July 2022. This change allows pharmacists to prescribe Paxlovid directly to people who have tested positive for COVID-19. This
means that you might be able to head over to your local pharmacy for the
medication without having to make other stops along the way. Keep in mind
that not all pharmacies may offer this service.
- Your current health records, which must be less than a year old (either electronic or printed records are fine)
- Your most recent liver and kidney function tests, which must be less than a year old
- A complete list of all medications that you take, including any over-the-counter (OTC) medications, vitamins, and supplements
How much will Paxlovid cost?
New Paxlovid Dose Pack Authorized by FDA
- The standard packaging that is currently in distribution: 300 mg nirmatrelvir;100 mg ritonavir - Each carton contains 30 tablets divided in 5 daily-dose blister cards. Each blister card contains 4 nirmatrelvir tablets (150 mg each) and 2 ritonavir tablets (100 mg each). Nirmatrelvir tablets and ritonavir tablets are supplied in separate blister cavities within the same child-resistant blister card.
- The new packaging option that will be in distribution later this month: 150 mg nirmatrelvir; 100 mg ritonavir - Each carton contains 20 tablets divided in 5 daily-dose blister cards. Each blister card contains 2 nirmatrelvir tablets (150 mg each) and 2 ritonavir tablets (100 mg each). Nirmatrelvir tablets and ritonavir tablets are supplied in separate blister cavities within the same child-resistant blister card.
Paxlovid for Long COVID
A June 2024 publication of The STOP-PASC Randomized Clinical Trial in JAMA, concluded that a 15-day course of Paxlovid in a population of patients with PASC (PostAcute Sequelae of SARS-CoV-2) infection was generally safe but did not demonstrate a significant benefit for improving select PASC symptoms (fatigue, brain fog, body aches, cardiovascular symptoms, shortness of breath, or gastrointestinal symptoms) in a mostly vaccinated cohort with protracted symptom duration. Further studies are needed to determine the role of Paxlovid in the treatment of Long COVID.Paxlovid Rebound
At the same time, the CDC wrote, “a brief return of symptoms may be part of the natural history of [coronavirus] infection in some persons, independent of treatment with Paxlovid and regardless of vaccination status.”
The CDC said there is no evidence for more treatment in rebound cases, though people should isolate again for at least 5 days so they won’t pass COVID-19 to others.
People who have a rebound after taking Paxlovid can report their cases to Pfizer’s adverse event reporting page.
Researchers found that when patients received a placebo instead of treatment, a portion of them still experienced a rebound of their symptoms after they had initially improved.
“Symptom return is common,” said Dr. Davey Smith, the chief of infectious diseases and global public health at the University of California, San Diego School of Medicine, who led the study. “It doesn’t mean that things are going south. It’s just the natural way the disease goes.” What is surprising, however, is how many people may experience a rebound, he said. (Read More)
How to treat rebound COVID after Paxlovid
Dr. Paul Auwaerter, head of Infectious Diseases at Johns Hopkins said:“I think when you're using drugs such as Paxlovid for only 5 days with one specific protease inhibitor, the nirmatrelvir component of the drug, it may be that that is not sufficient.”
Paxlovid's Contraindications and Drug Interactions
Pfizer anti-COVID pill's interaction with common drugs will narrow its benefit, experts say | National Post:
The buzz around PAXLOVID™ has largely obscured one major downside of this treatment. Ritonavir can interact dangerously with a slew of commonly used medications, pumping up the potency of blood thinners, heart-arrhythmia therapies, epilepsy drugs and others. And the patients targeted for its use – those most at risk of serious COVID disease because of age and other health issues – are also the people most likely to be taking those “contraindicated” medications.
In some cases, the interactions could be managed, but it’s clear the problem will limit the pool of potential recipients, experts say. “It has a utility, it has a use,” said Dr. Gerald Evans, head of the Infectious Diseases Division of the Queen’s University medical school. “(But) I certainly would not call it a game-changer.” “A patient on blood thinners could end up with spontaneous bleeding in the gastrointestinal tract or brain”, noted Evans.
“Someone taking pills for hypertension might see their blood pressure fall so much they pass out”, said Dr. Andrew Hill, a pharmacology researcher at the U.K.’s Liverpool University. “There are all kinds of ways that PAXLOVID™ could cause serious harm,” he said.
Ritonavir is also used in HIV treatments, so there is a wealth of knowledge about those potential drug interactions. The U.S. Food and Drug Administration (FDA) product monograph for PAXLOVID™ lists over 100 drugs that it says should not be taken with the COVID pills, or whose use ought to be carefully monitored. The figure below lists a few of these drugs as well as liver enzymes whose functions are impacted by Ritonavir.
See Sections 4 and 7 of the FACT SHEET FOR HEALTHCARE PROVIDERS and a publication on JAMA by Ross et al. Pharmacists as prescribers may be a problem since they are not authorized to manage, deprescribe and be responsible for the OTHER drugs.
There are many Paxlovid drug-interaction checkers, but the one we find most useful is from the University of Liverpool summarized in the Table below. For most, the interactions can be avoided by holding the 'medication of concern' until the 5-day treatment course is completed.

|
Molnupiravir and COVID-19
“I see this as an incredibly difficult decision with many more questions than answers,” said panel chair Dr. Lindsey Baden of Harvard Medical School, who voted in favor of the drug. He said FDA would have to carefully tailor the drug’s use for patients who stand to benefit most.
The recommendation came after hours of debate about the drug’s modest benefits and potential safety issues. Most experts backing the treatment stressed that it should not be used by anyone who is pregnant and called on FDA to recommend extra precautions before the drug is prescribed, such as pregnancy tests for women of child-bearing age.
Merck said final study results showed molnupiravir reduced hospitalization and death by 30% among adults infected with the coronavirus, when compared with adults taking a placebo. That effect was significantly less than the 50% reduction it first announced based on incomplete results.
For many panelists, the modest effect wasn’t enough to outweigh the drug’s potential toxicity to human fetuses.
“Given the large potential population affected, the risk of widespread effects on potential birth defects has not been adequately studied,” said Dr. Sankar Swaminathan of the University of Utah School of Medicine, who voted against the drug.
FDA scientists told the panelists earlier Tuesday that company studies in rats showed the drug caused birth defects when given at very high doses. FDA staffers concluded the data “suggest that molnupiravir may cause fetal harm when administered to pregnant individuals.”
The agency is weighing a blanket restriction against any use in pregnant women or allowing doctors to use the drug in rare cases. Some panelists said that option should be left open for pregnant mothers who have high-risk COVID-19 and may have few other treatment options.
Dr. Janet Cragan, who backed the drug, said that even with tight restrictions some pregnant women would inevitably take the antiviral.
“I don’t think you can ethically tell a woman with COVID-19 that she can’t have the drug if she’s decided that’s what she needs,” said Cragan, a panel member and staffer with the Centers for Disease Control and Prevention. “I think the final decision has to come down to the individual woman and her provider.”
Merck’s drug uses a novel approach to fight COVID-19: It inserts tiny errors into the coronavirus’ genetic code to stop it from reproducing. That genetic effect has raised concerns that the drug could spur more virulent strains of the virus. FDA regulators said Tuesday that risk is theoretical but many panelists said it should be carefully tracked in follow-up studies.
Antiviral pills have long been seen as a key advance beyond currently used antibody drugs, which must be injected or infused by health professionals. But given the shortcomings of Merck’s data, several experts said they would prioritize patients to receive the older drugs.
Ivermectin and COVID-19
- Ivermectin, antiviral properties and COVID-19: a possible new mechanism of action (Naunyn Schmiedebergs Arch Pharmacol. 2020).
- The multitargeted drug ivermectin: from an antiparasitic agent to a repositioned cancer drug (Am J Cancer Res. 2018)
Ivermectin Peer Reviewed and Other Studies
For a comprehensive review on ivermectin, please refer to the peer-reviewed publication; Review of the Emerging Evidence Supporting the Use of Ivermectin in the Prophylaxis and Treatment of COVID-19 and the included references.
Ivermectin and FLCCC's I-CARE Early Treatment Protocol
Based on rapidly emerging clinical trials evidence, the FLCCC team has developed the I-MASK+ protocol for prophylaxis and at home treatment of early stage COVID-19.
- Ivermectin has a number of potentially serious drug-drug interactions. Please check for potential drug interaction at Ivermectin Drug Interactions - Drugs.com. The most important drug interactions occur with cyclosporin, tacrolimus, anti-retroviral drugs, and certain anti-fungal drugs.
- Ivermectin is also lipophilic and therefore, bioavailability is maximised on a full stomach; or best to be taken with meal.
Ivermectin vs Molnupiravir
Retired nurse lecturer John Campbell, Ph.D., makes a critical comparison of the two in a YouTube video. To be upfront, Campbell says he is pro-vaccine and pro-antiviral.Ivermectin, he says, is one of the most-studied, repurposed drugs and, it’s not only FDA-approved for humans, but it won a Nobel prize as it “revolutionized the human treatment of a parasitic disease.” It also has demonstrated “broad spectrum antiviral activity against many viruses including HIV, Zika and MERS” and it inhibits the replication of the SARS coronavirus, and in fact got rid of 99.98% of SARS-viable particles in 48 hours.
Like ivermectin, molnupiravir is an oral drug, but it’s converted in the liver, and there is a safety concern that the metabolite action could also be mutagenic — cancerous — in mammalian cells as well as a trigger for birth defects in a fetus. While Merck says that’s not going to be a problem, Campbell says evidence he’s looking at shows “it at least needs looking into” because “if it stops the normal replication of RNA is it going to stop the normal replication of our DNA?”
Ivermectin, on the other hand, binds to the spike protein to stop it from going into your cells. It’s also an anti-inflammatory with high efficacy that inhibits cytokines and has very few side effects reported in its years of usage.
Paxlovid vs Molnupiravir vs Ivermectin
Is Paxlovid like Ivermectin? Clinical evidence to date has reported promising results for Ivermectin in prevention, early treatment as well as late treatment for COVID-19.Pfizer’s drug is part of a decades-old family of antiviral pills known as protease inhibitors, a standard treatment for HIV and hepatitis C. They work differently than Merck’s pill and haven’t been linked to the kind of mutation concerns raised with Merck’s drug.
According to AP News (Dec 1, 2021): Pfizer said that its drug shouldn’t be affected by the omicron variant’s mutations.Both drugs require patients to take multiple pills, twice a day for five days.The U.S. government has agreed to purchase 10 million treatment courses of Pfizer’s drug, if it’s authorized. That’s more than three times the government’s purchase agreement with Merck for 3.1 million courses of molnupiravir.
Key Takeaway
Z-Stack Supplement

The cost of the Z-STACK vitamin cocktail is $55 per bottle for a one month supply.
Note: To get 10% OFF, please use this coupon code: ONEDAYMD






.png)

Comments
Post a Comment